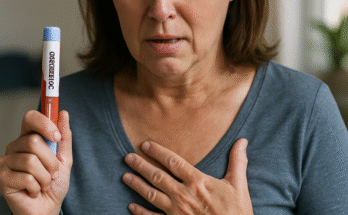
If you’re one of the millions of women navigating the challenges of polycystic ovary syndrome (PCOS), you’ve likely heard the buzz about Ozempic (semaglutide). This injectable drug, a superstar for type 2 diabetes and weight loss, is making waves for its potential to ease PCOS symptoms like insulin resistance and stubborn weight gain. But with a price tag of $800–$1,300 per month without coverage, the big question looms: Will my insurance cover Ozempic for PCOS? As an expert in healthcare policy and endocrinology, I’m here to guide you through the insurance maze, explain why coverage for PCOS is tricky, and share strategies to boost your chances of getting this game-changing drug covered. Let’s dive in!
Understanding PCOS and Ozempic’s Role
PCOS is a hormonal disorder affecting 6–20% of women of reproductive age, characterized by irregular periods, excess androgens (like testosterone), and, often, ovarian cysts. It’s a leading cause of infertility and comes with metabolic challenges, including insulin resistance in 35–80% of cases, which can lead to weight gain, prediabetes, and type 2 diabetes. According to the CDC, PCOS affects about 5 million women in the U.S. alone, many of whom struggle with weight management despite diet and exercise.
Enter Ozempic, a GLP-1 receptor agonist that mimics a hormone to regulate blood sugar, improve insulin sensitivity, slow digestion, and reduce appetite. While FDA-approved for type 2 diabetes and cardiovascular risk reduction, Ozempic is increasingly prescribed off-label for PCOS because it tackles insulin resistance and promotes weight loss—key to managing PCOS symptoms. A 2023 study of 27 obese PCOS patients found that low-dose Ozempic (0.5 mg weekly) led to an average weight loss of 7.6 kg and a BMI reduction of 3.1, with 78% losing at least 5% of their body weight. It also improved insulin resistance and menstrual regularity, making it a promising option.
But here’s the rub: Ozempic isn’t FDA-approved for PCOS, and that off-label status complicates insurance coverage. Let’s break down the factors at play.
Does Insurance Cover Ozempic for PCOS?
The answer is a frustrating maybe. Insurance coverage for Ozempic hinges on your diagnosis, your insurance provider, and the specifics of your plan. Here’s what you need to know:
- FDA Approval Matters: Ozempic is FDA-approved for type 2 diabetes and reducing cardiovascular risks in diabetic patients with heart disease. If you have PCOS and type 2 diabetes, most insurers, including UnitedHealthcare, Aetna, and Cigna, are likely to cover Ozempic for the diabetes indication. However, for PCOS alone, coverage is less likely because it’s an off-label use. Insurers often deem off-label prescriptions “experimental” or “investigational,” making denials common.
- Insurer Policies Vary: Major insurers like UnitedHealthcare, Aetna, and Blue Cross Blue Shield typically cover Ozempic for FDA-approved uses but are stingy with off-label ones. For example, a 2024 article notes that UnitedHealthcare may cover Ozempic for diabetes but not for PCOS or weight loss unless specific criteria are met. Some plans may cover Wegovy (a higher-dose semaglutide approved for weight loss) if you have obesity (BMI ≥30) or overweight (BMI 27–30) with comorbidities like insulin resistance, which is common in PCOS.
- Prior Authorization Is Key: Even if Ozempic is covered, insurers often require prior authorization (PA) for both diabetes and off-label uses. This means your doctor must submit documentation proving medical necessity, such as insulin resistance, failed attempts with other treatments (like metformin), or a high risk of type 2 diabetes. A 2024 Rescripted article suggests that having prediabetes or other risk factors alongside PCOS can strengthen your case for coverage.
- Medicare and Medicaid: If you’re on a Medicare Part D or Medicare Advantage plan, Ozempic is typically covered for type 2 diabetes but not for PCOS or weight loss. Medicaid coverage varies by state, and most states don’t cover Ozempic for off-label uses like PCOS due to strict formularies.
- Cost Without Coverage: Without insurance, Ozempic costs $800–$1,300 monthly, depending on your pharmacy and location. For PCOS patients without diabetes, this out-of-pocket cost can be a dealbreaker unless discounts or assistance programs are available.
Why Is Coverage for PCOS So Tricky?
The off-label hurdle is the biggest barrier. Since Ozempic lacks FDA approval for PCOS, insurers can deny coverage, arguing there’s insufficient evidence for its use in this condition. While studies, like the 2023 trial mentioned earlier, show benefits, they’re small-scale, and insurers often want large, randomized controlled trials before approving off-label coverage. A 2023 NBC News article notes that the evidence for Ozempic in PCOS lags behind patient experiences, with anecdotes outpacing rigorous clinical data.
Additionally, the high demand for Ozempic and other GLP-1 drugs (like Wegovy and Mounjaro) has led to shortages, making insurers stricter about approvals. Dr. Rekha Kumar, an endocrinologist quoted in 2023, said that inappropriate prescribing for weight loss has increased scrutiny, even for legitimate cases like PCOS with insulin resistance.
Strategies to Get Ozempic Covered for PCOS
Don’t let the complexity discourage you—there are ways to improve your odds of coverage:
- Work Closely with Your Doctor: Your healthcare provider is your biggest ally. They can build a strong case for medical necessity by documenting your PCOS symptoms (e.g., insulin resistance, irregular periods), failed treatments (like metformin), and risk factors like prediabetes. A 2024 article from Optum Perks emphasizes that detailed medical records can make or break a prior authorization request.
- Highlight Comorbidities: If you have prediabetes, obesity, or a high risk of type 2 diabetes, mention these to your doctor. Insurers are more likely to approve Ozempic if it’s tied to a covered condition. For example, a 2024 Rescripted article suggests that prediabetes alongside PCOS can bolster your case.
- Appeal Denials: If your insurer denies coverage, don’t give up. File an appeal with additional evidence, such as studies on Ozempic’s benefits for PCOS (e.g., the 2023 study showing weight loss and insulin improvements) or a letter from an endocrinologist. Patient advocacy groups for PCOS can also provide resources for navigating appeals.
- Explore Alternatives: If Ozempic isn’t covered, ask about Wegovy or Mounjaro, which may be approved for weight loss in patients with obesity or insulin resistance. A 2024 article from Illume Fertility notes that Wegovy, which contains semaglutide, is FDA-approved for weight loss, potentially making it easier to get covered for PCOS-related weight issues.
- Use Discount Programs: If coverage isn’t an option, programs like GoodRx or SingleCare can lower costs to $900–$1,000 monthly. Novo Nordisk’s Patient Assistance Program may also help if you meet income criteria. Compounded semaglutide, available through some clinics, can cost less (e.g., $999 for 3 months) but isn’t FDA-approved and carries risks.
Real-World Insights
On platforms like X and Reddit, PCOS patients share mixed experiences. One user in 2024 reported getting Ozempic covered by Cigna for PCOS with prediabetes after a detailed PA, while another was denied by Aetna because PCOS wasn’t an approved indication. Another user noted a $1,200 monthly cost without coverage, prompting them to switch to compounded semaglutide. These stories highlight the variability and the need for persistence.
The Future of Ozempic for PCOS
The good news? Research is growing. Studies like the 2023 trial and ongoing clinical trials (e.g., on ClinicalTrials.gov) are exploring GLP-1 agonists for PCOS, which could lead to FDA approval and broader insurance coverage in the future. As awareness of PCOS grows, insurers may also loosen restrictions, especially if larger trials confirm benefits.
FAQs
- Will insurance cover Ozempic for PCOS if I don’t have diabetes?
Coverage for Ozempic for PCOS alone is unlikely since it’s not FDA-approved for this use. Insurers often deny off-label prescriptions, but you may qualify if you have prediabetes or obesity. Work with your doctor to document medical necessity and appeal denials with evidence like studies showing Ozempic’s benefits for PCOS. - What can I do if my insurance denies Ozempic for PCOS?
File an appeal with your doctor’s help, providing documentation of insulin resistance, failed treatments (e.g., metformin), or prediabetes. Alternatively, ask about covered GLP-1 drugs like Wegovy for weight loss. Discount programs like GoodRx or Novo Nordisk’s Patient Assistance Program can also reduce costs if coverage isn’t granted. - How much does Ozempic cost without insurance for PCOS?
Without insurance, Ozempic costs $800–$1,300 monthly, depending on your pharmacy. Discount programs can lower this to $900–$1,000. Compounded semaglutide may cost less (e.g., $999 for 3 months) but isn’t FDA-approved. Check with your doctor and explore assistance programs to manage costs.
The Bottom Line
Getting insurance to cover Ozempic for PCOS is an uphill battle due to its off-label status, but it’s not impossible. If you have type 2 diabetes or prediabetes alongside PCOS, your chances are higher, especially with a strong prior authorization. Without these conditions, you may face denials and need to appeal or explore alternatives like Wegovy. Work closely with your doctor, gather supporting evidence, and consider discount programs if coverage isn’t an option. PCOS is tough, but with persistence and the right strategy, you can access treatments like Ozempic to manage symptoms and reclaim your health. Stay in the fight!

Lisa Caldwell is a clinical health writer and certified diabetes educator with a strong background in pharmacology and metabolic health. With over 12 years of experience in patient education, she specializes in translating complex research on GLP-1 medications like Ozempic into clear, practical guidance.