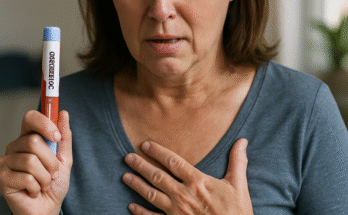
Weight loss is a journey that often feels like navigating a maze—full of twists, turns, and tempting shortcuts. For those struggling to shed pounds, medications like Ozempic and phentermine have emerged as powerful tools, each with its own strengths. Ozempic, a GLP-1 receptor agonist, is celebrated for its ability to regulate blood sugar and curb appetite, while phentermine, a stimulant, is a go-to for short-term appetite suppression. But what happens when you consider combining these two? Can you take phentermine with Ozempic safely and effectively? As an expert in pharmacology and weight management, I’m here to unpack the science, risks, and potential benefits of this combination, helping you make informed decisions about your health.
Phentermine: The Classic Appetite Suppressant
Phentermine, a stimulant similar to amphetamines, has been a staple in weight loss treatment since the 1950s. Approved for short-term use (typically 12 weeks), it works by boosting norepinephrine levels in the brain, suppressing appetite, and increasing energy expenditure. Patients often report rapid weight loss—5-10% of body weight in a few months—but it’s not without drawbacks. Side effects include increased heart rate, elevated blood pressure, insomnia, and potential for dependence, which is why it’s tightly regulated as a Schedule IV controlled substance. Phentermine is typically prescribed for those with a BMI over 30 or 27 with weight-related conditions, but its short-term nature leaves many wondering about longer-term solutions, like combining it with Ozempic.
Why Consider Combining Phentermine and Ozempic?
The idea of combining phentermine and Ozempic is appealing because they target weight loss differently. Phentermine offers a quick, intense appetite suppression, ideal for jump-starting weight loss, while Ozempic provides sustained appetite control and metabolic benefits. Some patients and doctors theorize that pairing them could amplify results—phentermine’s rapid action could kickstart the process, while Ozempic supports long-term weight maintenance. This combination is particularly tempting for those who’ve hit a plateau with one drug or need faster results. However, the question isn’t just whether it works—it’s whether it’s safe and medically sound.
The Science Behind Combining Phentermine and Ozempic
No large-scale clinical trials have directly studied the combination of phentermine and Ozempic, so we rely on pharmacological principles and anecdotal evidence. Both drugs suppress appetite, but their mechanisms don’t directly overlap. Phentermine stimulates the central nervous system, increasing heart rate and alertness, while Ozempic works peripherally, slowing digestion and signaling fullness to the brain. This complementary action suggests potential synergy, but it also raises concerns about additive side effects. For example, phentermine’s cardiovascular effects (elevated heart rate and blood pressure) could compound Ozempic’s milder cardiovascular impact, potentially stressing the heart. Additionally, both drugs can cause gastrointestinal issues—nausea from Ozempic and dry mouth or constipation from phentermine—which could make the combination uncomfortable for some.
Safety Concerns and Risks
Safety is the biggest hurdle when considering this combination. Phentermine’s stimulant properties make it unsuitable for patients with heart conditions, high blood pressure, or anxiety disorders. Ozempic, while generally safer for long-term use, carries risks like pancreatitis, gallbladder issues, and, in rare cases, thyroid cancer. Combining them could amplify these risks, particularly for those with pre-existing conditions. For instance, a 2023 case report described a patient experiencing elevated heart rate and palpitations when combining the two, though they achieved significant weight loss. Drug interactions are another concern—while no direct interactions between phentermine and Ozempic are documented, both can affect blood sugar and blood pressure, requiring careful monitoring. The lack of long-term data means doctors must rely on clinical judgment, making medical supervision critical.
What Do Doctors Say About Combining These Medications?
Most healthcare providers approach this combination with caution. Endocrinologists and obesity specialists may consider it for carefully selected patients—those with significant obesity, no cardiovascular issues, and a history of poor response to single-drug therapy. A typical approach might involve starting with Ozempic to establish tolerability, then adding low-dose phentermine for a short period (e.g., 8-12 weeks) to boost weight loss. Regular monitoring of blood pressure, heart rate, and blood sugar is essential. Some clinics, like those specializing in medical weight loss, report success with this strategy, but it’s not standard practice. The American Association of Clinical Endocrinologists emphasizes individualized treatment plans, warning against combining medications without clear medical rationale.
Patient Experiences: Anecdotes from the Field
Patient stories offer a glimpse into the real-world use of this combination. On forums like Reddit, users report mixed experiences. One woman in her 40s shared that combining low-dose phentermine with Ozempic helped her lose 20 pounds in two months, far surpassing her results with Ozempic alone. However, she noted increased anxiety and difficulty sleeping, side effects she attributed to phentermine. Another user reported nausea and palpitations, forcing them to stop the combination. These anecdotes highlight the variability of responses and the need for personalized medical guidance. What works for one person may be intolerable for another, underscoring the importance of working closely with a healthcare provider.
Alternatives to Combining Phentermine and Ozempic
Before jumping to combination therapy, consider alternatives. Optimizing Ozempic with lifestyle changes—diet, exercise, and behavioral therapy—can yield impressive results without the risks of adding phentermine. Other GLP-1 agonists, like Wegovy (a higher-dose semaglutide approved specifically for weight loss), may offer similar benefits with a better safety profile for long-term use. For those needing a phentermine-like boost, newer medications like Qsymia (a phentermine-topiramate combination) provide a controlled-release option with potentially fewer side effects. Consulting a weight loss specialist can help identify the best approach for your needs.
Practical Tips for Those Considering the Combination
If you and your doctor decide to explore combining phentermine and Ozempic, start with a thorough medical evaluation to rule out contraindications like heart disease or uncontrolled hypertension. Begin with the lowest effective doses—phentermine is often prescribed at 15-37.5 mg daily, while Ozempic starts at 0.25 mg weekly. Monitor side effects closely, especially in the first few weeks, and keep a log of symptoms like heart rate changes or gastrointestinal discomfort. Stay hydrated, as both drugs can cause dehydration. Most importantly, don’t self-medicate—obtaining either drug without a prescription (e.g., through unregulated sources) is risky and illegal. Regular follow-ups with your doctor ensure the combination remains safe and effective.
Frequently Asked Questions
Can everyone take phentermine and Ozempic together?
Not everyone is a candidate for this combination. It’s generally considered for patients with significant obesity and no contraindications like heart disease, high blood pressure, or anxiety disorders. A thorough medical evaluation is essential to assess risks, and the combination should only be used under close medical supervision due to potential side effects like elevated heart rate or gastrointestinal issues.
How long can you safely combine phentermine and Ozempic?
Phentermine is approved for short-term use, typically 8-12 weeks, due to its stimulant properties and risk of dependence. Ozempic can be used long-term for diabetes or weight management. If combined, doctors usually limit phentermine’s duration to avoid cardiovascular strain or tolerance, while Ozempic may continue for sustained benefits. Your doctor will tailor the timeline based on your progress and health.
What should I do if I experience side effects from the combination?
If you experience side effects like rapid heart rate, severe nausea, or anxiety, contact your doctor immediately. They may adjust the dose, discontinue one medication, or recommend alternatives. Keep a symptom log to help your doctor assess whether the combination is safe for you, and never stop either drug abruptly without medical guidance.
Conclusion: Proceed with Caution and Expertise
Combining phentermine and Ozempic holds promise for some, offering a dual approach to appetite suppression and weight loss. However, the lack of large-scale studies and potential for serious side effects mean it’s not a one-size-fits-all solution. With careful medical supervision, personalized dosing, and vigilant monitoring, this combination could be a game-changer for those struggling with obesity. But it’s not a DIY project—work closely with your doctor to weigh the benefits against the risks. Whether you choose this path or explore alternatives, the journey to better health is about informed choices, persistence, and partnership with your healthcare team.

Lisa Caldwell is a clinical health writer and certified diabetes educator with a strong background in pharmacology and metabolic health. With over 12 years of experience in patient education, she specializes in translating complex research on GLP-1 medications like Ozempic into clear, practical guidance.