You’re scrolling through social media, seeing transformation photos left and right. Everyone’s talking about Ozempic – that weekly injection that’s the holy grail of weight loss. But then you stumble across a comment that makes you pause: “Wait, can Ozempic cause blood clots?”
Look, I’ve been down this rabbit hole myself. When my doctor first mentioned Ozempic for my type 2 diabetes, I thought I’d hit the jackpot – better blood sugar AND weight loss? Sign me up. But then I started digging deeper into the research, and honestly, the blood clot question kept me up at night.
Here’s what I wish someone had told me straight up, without all the medical jargon and corporate speak.
The Real Talk on Ozempic and Blood Clots
Can Ozempic cause blood clots? The short answer: it’s complicated, and the research shows mixed signals that’ll make your head spin.
Recent studies have put this question front and center, especially with ongoing litigation bringing more scrutiny to semaglutide’s circulatory effects. But here’s where it gets interesting – the data points in two completely different directions.
On one hand, some clinical trials found a 266% increased incidence of venous thromboembolism (VTE) – that’s deep vein thrombosis and pulmonary embolism – in diabetic patients using semaglutide compared to placebo groups. Yeah, that number sounds scary as hell.
But flip the coin, and a massive 2024 study of 558,000 patients showed GLP-1 medications might actually lower clot risk by 20% compared to other diabetes drugs. The researchers found 6.5 versus 7.9 events per 1,000 patient-years.
So which is it? Your guess is as good as mine – and that’s exactly the problem.
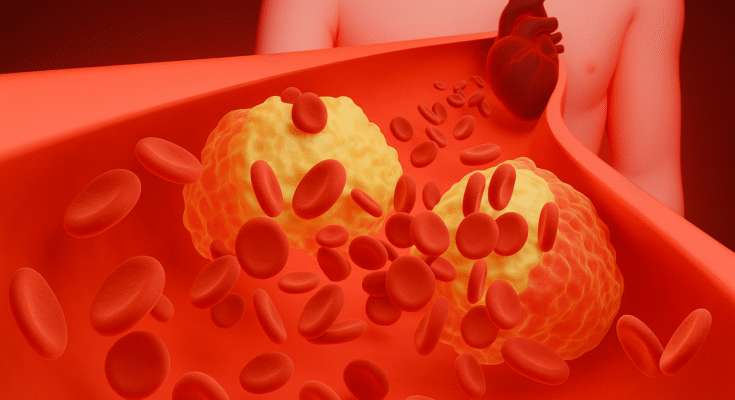
Why Your Body Might Form Clots on Ozempic
The mechanism behind potential blood clots isn’t some random side effect – there are actually several biological pathways that make sense when you think about how Ozempic works.
The Dehydration Factor
This is the big one nobody talks about enough. Ozempic slows down your stomach’s emptying process, which sounds great for appetite control. But it also cranks up your chances of nausea, vomiting, and diarrhea – we’re talking a 166% increased incidence of GI issues.
When you’re constantly dealing with these side effects, dehydration becomes your new best friend. And dehydrated blood? It gets thick and sticky, exactly the consistency that loves forming clots.
I learned this the hard way during my first month on Ozempic. I was so focused on the appetite suppression that I barely noticed I wasn’t drinking enough water. My lips were constantly chapped, and I felt dizzy when standing up. Looking back, those were red flags I should’ve caught earlier.
The Inflammation Curveball
Here’s something that blew my mind: while Ozempic reduces overall body fat (which should lower inflammation), the acute weight loss process might temporarily spike inflammatory markers like C-reactive protein. These inflammatory signals can actually stimulate your body’s clotting pathways.
Think of it like renovating your house – the end result is beautiful, but the construction phase is messy and chaotic.
The Mobility Issue
Semaglutide can reduce lean muscle mass by up to 14% in some studies. Less muscle means less movement, and less movement means blood that sits around longer in your veins. That stagnant blood? Prime real estate for clot formation.
Who’s Actually at Risk?
Not everyone faces the same blood clot risk on Ozempic. The research shows certain groups need to pay extra attention.
High-Risk Categories
If you’ve got a BMI over 35 with a history of blood clots, you’re in the high-risk club. The combination of obesity-related inflammation plus Ozempic’s potential effects creates a perfect storm scenario.
Diabetics with autonomic neuropathy face amplified risks because their blood vessels can’t react properly to dehydration. Your body’s usual “hey, we need more fluid” signals just don’t work the same way.
Limited mobility patients get hit with a double whammy – existing circulation issues plus potential muscle loss from the medication.
The Medication Cocktail Problem
Taking birth control or corticosteroids while on Ozempic? These combinations might synergistically elevate your thrombosis potential. Your pharmacist should flag these interactions, but honestly, double-check everything yourself.
What to Watch For (Beyond the Obvious)
Forget the generic “call your doctor if you experience unusual symptoms” advice. Here’s what actually matters when monitoring for blood clots on Ozempic.
Early Warning Signs
Leg pain that won’t quit – especially if it’s in your calf and gets worse when you flex your foot upward. This isn’t your typical workout soreness.
Sudden shortness of breath that hits you out of nowhere, even during simple activities like walking to the mailbox.
Chest pain that feels different – not the crushing heart attack type, but more like a sharp, stabbing sensation that gets worse when you breathe deeply.
The Monitoring Game Plan
Your doctor should be tracking specific markers, not just asking “how are you feeling?” Complete blood counts help catch dehydration-induced blood thickening before it becomes a problem.
D-dimer levels above 500 ng/mL warrant ultrasound screening. If your healthcare provider isn’t familiar with this protocol, find someone who is.
The Real-World Risk Assessment
Let me break down the numbers without the statistical gymnastics that make your eyes glaze over.
| Risk Factor | Baseline VTE Risk | Potential Ozempic Impact |
| Healthy adults | 1-2 per 1,000 people/year | Potentially unchanged or slightly lower |
| Type 2 diabetics | 2-4 per 1,000 people/year | Mixed data: possibly higher short-term, lower long-term |
| High-risk patients (BMI >35 + prior VTE) | 10-20 per 1,000 people/year | Requires individualized assessment |
The bottom line? For most people considering Ozempic, the absolute risk remains relatively low. But “relatively low” doesn’t mean zero, and it definitely doesn’t mean you can ignore the warning signs.
Smart Strategies for Staying Safe
If you’re moving forward with Ozempic despite the blood clot concerns, here’s how to stack the deck in your favor.
Hydration That Actually Works
Skip the “drink 8 glasses of water” nonsense. When you’re dealing with Ozempic’s GI effects, you need electrolyte replacement that matches what you’re losing. Oral rehydration solutions containing 20-30 mEq/L of potassium and 60-70 mEq/L of sodium work better than plain water.
Movement That Matters
Resistance training 2-3 times per week isn’t just about aesthetics – it’s about maintaining the muscle mass that keeps your blood flowing properly. Even bodyweight exercises beat sitting on the couch scrolling TikTok.
The Compression Game
20-30 mmHg graduated compression stockings during your dose titration phases can be a game-changer, especially if you’re spending long hours at a desk job.
When the Risk-Benefit Math Gets Tricky
Here’s where I’ll be brutally honest: the decision to start Ozempic knowing about potential blood clot risks isn’t black and white.
For diabetics dealing with obesity, the cardiovascular benefits often outweigh the VTE risks, especially with proper monitoring and mitigation strategies in place.
For non-diabetic weight loss seekers, the math gets murkier. You’re potentially accepting unknown risks for aesthetic benefits, particularly if you have any inherited blood clotting disorders lurking in your family tree.
I’ve watched friends make both choices – some decided the potential risks weren’t worth it, others felt the benefits justified careful monitoring. Both decisions were valid based on their individual circumstances.
FAQ’s
When should I be worried about Ozempic side effects?
You can help prevent or reduce some unpleasant symptoms by avoiding high-fat foods, greasy or fried foods, and sweets. Most side effects of Ozempic aren’t serious, but you should see a doctor right away if you have: Prolonged or severe diarrhea or throwing up. Intense pain or tenderness in your belly.
What happens when you first start Ozempic?
What to Expect After Your First Ozempic Injection. It’s normal to experience some side effects from a new medication. According to Dr. Ali, the most common side effects reported from Ozempic are gastrointestinal, such as nausea, diarrhea or constipation, stomach cramping, and vomiting.
How do I know if Ozempic is affecting my pancreas?
Symptoms of Pancreatitis While On Ozempic. Doctors can diagnose acute pancreatitis by checking for high levels of pancreatic enzymes (like lipase or amylase) in your blood. They may also use imaging tests, like a CT scan or MRI, to look for inflammation caused by acute pancreatitis.
How do you know if you have a blood clot?
Blood clot symptoms. Arms and legs: Pain or tenderness, swelling, or warm feeling. Brain: Trouble speaking; vision changes; sudden, strong headache; dizziness; or weakness in face, arms, or legs. Heart: Pain in the chest or other part of the upper body, breathing difficulties, sweating, nausea, or light-headedness.
The Bottom Line on Ozempic and Blood Clots
Can Ozempic cause blood clots? The research suggests it’s possible through several biological mechanisms, but the clinical significance varies dramatically between individuals.
The conflicting study results tell us we’re still figuring this out. What we know for certain is that dehydration, reduced mobility, and inflammatory changes can all contribute to clot formation – and Ozempic potentially influences all three factors.
Your move? If you’re seriously considering Ozempic, find a healthcare provider who understands these nuances and won’t just hand you a prescription with a pat on the head. Someone who’ll monitor the right markers, recognize early warning signs, and adjust your treatment plan based on your individual risk profile.
The weight loss medication landscape is evolving rapidly, and the safety data is still catching up to the hype. Making an informed decision means acknowledging both the potential benefits and the legitimate concerns – including the blood clot question that brought you here in the first place.
Don’t let fear paralyze you, but don’t let desperation for quick results blind you to real risks either. Your health is worth the extra research and careful consideration.
Emily Harper is a board-certified nurse practitioner and certified obesity medicine specialist with a strong clinical background in metabolic health and GLP-1 therapies. With years of frontline experience managing patients on Ozempic, she brings both scientific knowledge and real-world insight to her writing.