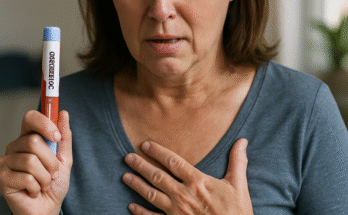
If you’re taking Ozempic and have surgery scheduled, you’re probably wondering when to stop taking your medication. The timing is crucial for your safety during the procedure, and recent medical guidelines provide clear recommendations that can help protect you from serious complications.
The Quick Answer: Current Medical Guidelines
The American Society of Anesthesiologists (ASA) said in a recent statement that people who take the GLP-1 agonists every day should stop the medication on the day of the surgery. If the person takes the medicine weekly, they should hold it a week before the surgery. However, newer research suggests that these guidelines may be evolving, and the timing may depend on your individual circumstances and the type of procedure you’re having.
Why Stopping Ozempic Before Surgery Is Important
Understanding why you need to stop Ozempic before surgery helps you appreciate the importance of following your doctor’s instructions. Based on recent anecdotal reports, there are concerns that delayed gastric emptying from GLP-1 agonists can increase the risk of regurgitation and pulmonary aspiration of gastric contents during general anesthesia and deep sedation. This means that food or stomach contents could potentially enter your lungs during surgery, which can lead to serious complications including pneumonia.
Ozempic works by slowing down how quickly your stomach empties, which is part of how it helps with weight loss and blood sugar control. While this mechanism is beneficial for managing diabetes and weight, it creates a safety concern during surgery because your stomach may still contain food or liquid even after fasting.
Current Medical Guidelines and Recommendations
The medical community has developed specific guidelines for stopping Ozempic and other GLP-1 medications before surgery. For elective procedures, the group recommends that patients who take a daily dose of a GLP-1 drug should hold the treatment the day of surgery, and those who take a weekly dose should hold it the week before surgery.
However, some medical professionals recommend a more conservative approach. According to president of the American Society of Anesthesiologists, it’s imperative to stop taking Ozempic (as well as other forms of semaglutide) at least two weeks prior to your surgical date. This longer timeframe allows more time for the medication’s effects on stomach emptying to diminish.
Recent Changes in Medical Thinking
The medical understanding of GLP-1 medications and surgery is evolving rapidly. Doctors may not need to require patients discontinue GLP-1 agonists such as Wegovy and Ozempic for seven days before any surgery or endoscopy, according to a Houston Methodist Hospital-led study. This emerging research suggests that the blanket recommendation to stop all GLP-1 medications may not be necessary for every patient.
Patients in the escalation phase of GLP-1 drugs (early in treatment) are more likely to have delayed stomach emptying. The escalation phase (when the patient is given increasing doses of the GLP-1 drug) typically lasts four to eight weeks, depending on the drug and the reason it has been prescribed. This means that if you’ve recently started Ozempic or are still adjusting your dose, your doctor may recommend stopping the medication for a longer period before surgery.
Types of Surgery and Different Considerations
Not all surgeries require the same approach to stopping Ozempic. Emergency surgeries obviously don’t allow time for medication adjustments, so your medical team will need to take special precautions during the procedure. For elective surgeries, you have the advantage of planning ahead and following the recommended timeline for stopping your medication.
The type of anesthesia you’ll receive also matters. Procedures requiring only local anesthesia may not require stopping Ozempic at all, while those requiring general anesthesia or deep sedation carry higher risks and typically require medication cessation. Your anesthesiologist will work with your surgeon and primary care physician to determine the best approach for your specific situation.
Signs You May Need Extra Precautions
The presence of adverse gastrointestinal symptoms (nausea, vomiting, dyspepsia, abdominal distension) in patients taking GLP-1 agonists are predictive of increased residual gastric contents. If you’re experiencing these symptoms while taking Ozempic, it’s especially important to discuss this with your surgical team, as you may need additional precautions or a longer medication-free period before surgery.
People who have been taking Ozempic for a shorter time may also need extra consideration. The medication’s effects on stomach emptying are typically stronger when you first start taking it and may decrease over time as your body adjusts. If you’ve been taking Ozempic for less than a few months, your doctor might recommend stopping it earlier before surgery.
Managing Diabetes During the Medication Break
If you’re taking Ozempic for diabetes management, stopping the medication before surgery doesn’t mean abandoning your blood sugar control. Those taking the drugs to control diabetes might need to briefly switch to another drug. Your endocrinologist or primary care physician can help you develop a plan to manage your blood sugar during the time you’re not taking Ozempic.
This might involve temporary insulin therapy, other oral diabetes medications, or careful dietary management. The key is working with your healthcare team to ensure your blood sugar remains stable while prioritizing your safety during surgery.
What to Expect After Surgery
The good news is that you typically don’t have to wait long after surgery to resume your Ozempic. Patients can resume taking their GLP-1 agonist the next day after surgery. However, this depends on several factors including how well you’re recovering, whether you’re able to eat and drink normally, and what your surgical team recommends.
Some people may need to start with a lower dose when resuming Ozempic after a break, especially if they’ve been off the medication for more than a week. This can help minimize side effects like nausea and vomiting as your body readjusts to the medication.
Special Considerations for Different Procedures
Certain types of procedures may require different approaches to stopping Ozempic. Gastrointestinal procedures, for example, might require a longer medication-free period because they directly involve the digestive system where Ozempic has its primary effects.
Cosmetic procedures and outpatient surgeries still require the same precautions as major surgeries if they involve general anesthesia. The risk of aspiration exists regardless of whether the surgery is considered major or minor, so don’t assume that a “simple” procedure means you can continue taking Ozempic.
Working with Your Healthcare Team
The most important step in managing Ozempic before surgery is clear communication with all members of your healthcare team. Make sure your surgeon, anesthesiologist, and the physician who prescribed your Ozempic all know about your medication and surgical plans.
Don’t stop taking Ozempic without medical supervision, especially if you’re using it for diabetes management. Your healthcare providers need to coordinate your care to ensure both your surgical safety and your ongoing health management are addressed.
Questions to Ask Your Medical Team
When preparing for surgery while taking Ozempic, consider asking your healthcare providers several important questions. Find out exactly when you should stop taking your medication and whether you need any alternative treatments during the break. Ask about signs or symptoms that might indicate complications and what you should do if you experience them.
It’s also important to understand when you can safely resume Ozempic after surgery and whether you’ll need to restart at a lower dose. Discuss how your diabetes management will be handled during the medication break and what monitoring might be necessary.
Emergency Surgery Considerations
If you need emergency surgery while taking Ozempic, your medical team will need to take special precautions. They may use rapid sequence intubation techniques and other methods to protect your airway during anesthesia. While this situation is more complex, experienced anesthesiologists are trained to handle these scenarios safely.
The key in emergency situations is making sure your medical team knows you’re taking Ozempic so they can adjust their approach accordingly. Always carry information about your medications or keep it easily accessible for emergency situations.
The Bottom Line
The current medical consensus suggests stopping Ozempic one week before surgery if you take it weekly, or on the day of surgery if you take a daily GLP-1 medication. However, some physicians recommend a more conservative two-week break, especially for patients who are newer to the medication or experiencing gastrointestinal symptoms.
The most important thing is working closely with your healthcare team to develop a plan that’s right for your specific situation. Every patient is different, and factors like how long you’ve been taking Ozempic, why you’re taking it, what type of surgery you’re having, and your overall health all influence the best approach.
Recent research suggests that these guidelines may continue to evolve as we learn more about GLP-1 medications and surgical safety. What remains constant is the importance of open communication with your healthcare providers and following their specific recommendations for your situation.
Remember that stopping Ozempic temporarily before surgery is about ensuring your safety during the procedure. With proper planning and medical supervision, you can safely navigate this temporary interruption in your treatment while maintaining your overall health and achieving your surgical goals.

James Rowen is a certified medical writer and healthcare researcher specializing in endocrinology and metabolic health. With over a decade of experience analyzing weight management therapies, James has developed deep expertise in GLP-1 receptor agonists, including Ozempic.