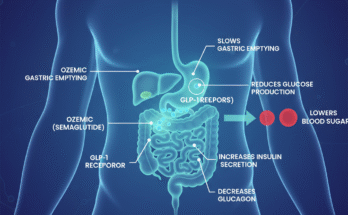
Understanding Ozempic (semaglutide) and its safety profile has become increasingly important as more people with various health conditions, including breast cancer patients and survivors, consider this medication for diabetes management and weight loss. This glucagon-like peptide-1 (GLP-1) receptor agonist works by mimicking natural hormones in your body that regulate blood sugar levels and appetite control.
The medication belongs to a class of drugs called GLP-1 agonists, which also includes medications like Wegovy, Mounjaro, and Trulicity. These pharmaceutical agents have revolutionized diabetes care and weight management, but their use in oncology patients raises important questions about drug interactions, treatment safety, and potential risks.
Understanding Breast Cancer and Weight Management Connection
Breast cancer remains one of the most common malignancies affecting women worldwide, though men can develop it too. This disease occurs when abnormal cells in breast tissue grow uncontrollably, forming tumors that can spread to other parts of the body. Cancer treatment typically involves a combination of surgery, radiation therapy, chemotherapy, hormone therapy, or targeted biological therapies, depending on the cancer stage and specific tumor characteristics.
Many breast cancer patients experience weight gain during and after treatment, which can be attributed to hormonal changes, reduced physical activity, chemotherapy effects, and certain medications like corticosteroids or hormone blockers such as tamoxifen and aromatase inhibitors. This weight gain isn’t just a cosmetic concern—it can impact treatment outcomes, increase recurrence risk, and affect overall quality of life.
Maintaining a healthy body weight plays a crucial role in cancer prevention and survivorship. Research has consistently shown that obesity is associated with increased breast cancer risk, particularly in postmenopausal women. Excess body fat leads to elevated estrogen levels, chronic inflammation, insulin resistance, and metabolic dysfunction—all factors that can promote tumor growth and progression.
For cancer survivors, weight management becomes even more critical. Studies indicate that women who gain significant weight after breast cancer diagnosis may face higher recurrence rates and poorer survival outcomes. Conversely, maintaining optimal body composition through proper nutrition and regular physical activity can improve prognosis, reduce treatment-related side effects, and enhance overall wellbeing.
Safety of Ozempic for Breast Cancer Patients
The question of whether breast cancer patients can take Ozempic doesn’t have a simple yes or no answer. The safety and appropriateness depend on multiple factors including cancer stage, current treatment status, overall health condition, and individual risk factors.
Clinical trials of semaglutide have not demonstrated an increased risk of breast cancer development. The medication primarily affects blood glucose regulation and satiety signals in the brain, mechanisms that don’t directly interact with breast tissue or hormone receptors typically involved in breast malignancies.
However, it’s essential to understand that Ozempic carries a boxed warning about thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), based on animal studies. While this thyroid cancer risk hasn’t been confirmed in humans, patients with personal or family history of MTC or multiple endocrine neoplasia syndrome type 2 (MEN 2) should avoid this medication entirely.
Using Ozempic During Active Cancer Treatment
Using Ozempic during active chemotherapy, radiation, or immunotherapy requires careful medical supervision. The medication can cause gastrointestinal side effects including nausea, vomiting, diarrhea, and decreased appetite—symptoms that may overlap with or exacerbate treatment-related adverse effects. Cancer patients undergoing aggressive therapies need adequate nutritional intake to maintain strength, support healing, and tolerate treatment protocols.
Healthcare providers typically evaluate several factors before prescribing GLP-1 medications to active cancer patients. Nutritional status is paramount—patients already experiencing treatment-related weight loss or malnutrition may not be suitable candidates, as the appetite-suppressing effects could worsen these conditions. Those in maintenance phases or who have completed active treatment may be better candidates than those currently receiving intensive chemotherapy or radiation.
Gastrointestinal function is another critical consideration. Pre-existing digestive issues could be worsened by semaglutide’s effects on gastric emptying and intestinal motility. Additionally, Ozempic can affect the absorption of oral medications, which is particularly relevant for patients taking multiple drugs as part of their cancer care regimen.
Benefits of Ozempic for Breast Cancer Survivors

For breast cancer survivors who have completed treatment, the considerations differ from those in active therapy. Many survivors struggle with weight gain from hormone therapy, reduced metabolism, and lifestyle changes during treatment. For these individuals, GLP-1 receptor agonists might offer significant benefits.
Semaglutide has demonstrated remarkable efficacy in promoting weight reduction, with clinical trials showing average weight loss of 15-20% of body weight. For survivors carrying excess weight, this could potentially reduce recurrence risk and improve cardiovascular health. Many cancer survivors develop insulin resistance or type 2 diabetes, particularly after certain treatments. Ozempic addresses both conditions simultaneously, offering dual benefits for metabolic syndrome management.
Recent studies show that GLP-1 agonists provide cardiovascular benefits beyond glucose control and weight loss, reducing risk of heart attacks and strokes—important considerations since cancer survivors face elevated cardiovascular disease risk. Chronic low-grade inflammation contributes to both obesity and cancer progression. Semaglutide has anti-inflammatory properties that may benefit overall health and potentially reduce cancer recurrence risk, though more research is needed in this area.
Important Contraindications and Precautions
Despite potential benefits, certain breast cancer survivors should exercise caution or avoid Ozempic entirely. While no direct interaction exists between semaglutide and hormone receptor-positive breast cancers, patients on endocrine therapy should discuss potential drug interactions with their oncologist.
Those with strong family histories of thyroid cancer or MEN 2 syndrome should not use this medication due to the thyroid tumor warning. Patients with history of pancreatitis, severe gastroparesis, or inflammatory bowel disease need careful evaluation before starting GLP-1 therapy. Semaglutide requires dose adjustment in patients with renal impairment, and severe kidney disease may contraindicate its use.
Current Research and Clinical Studies
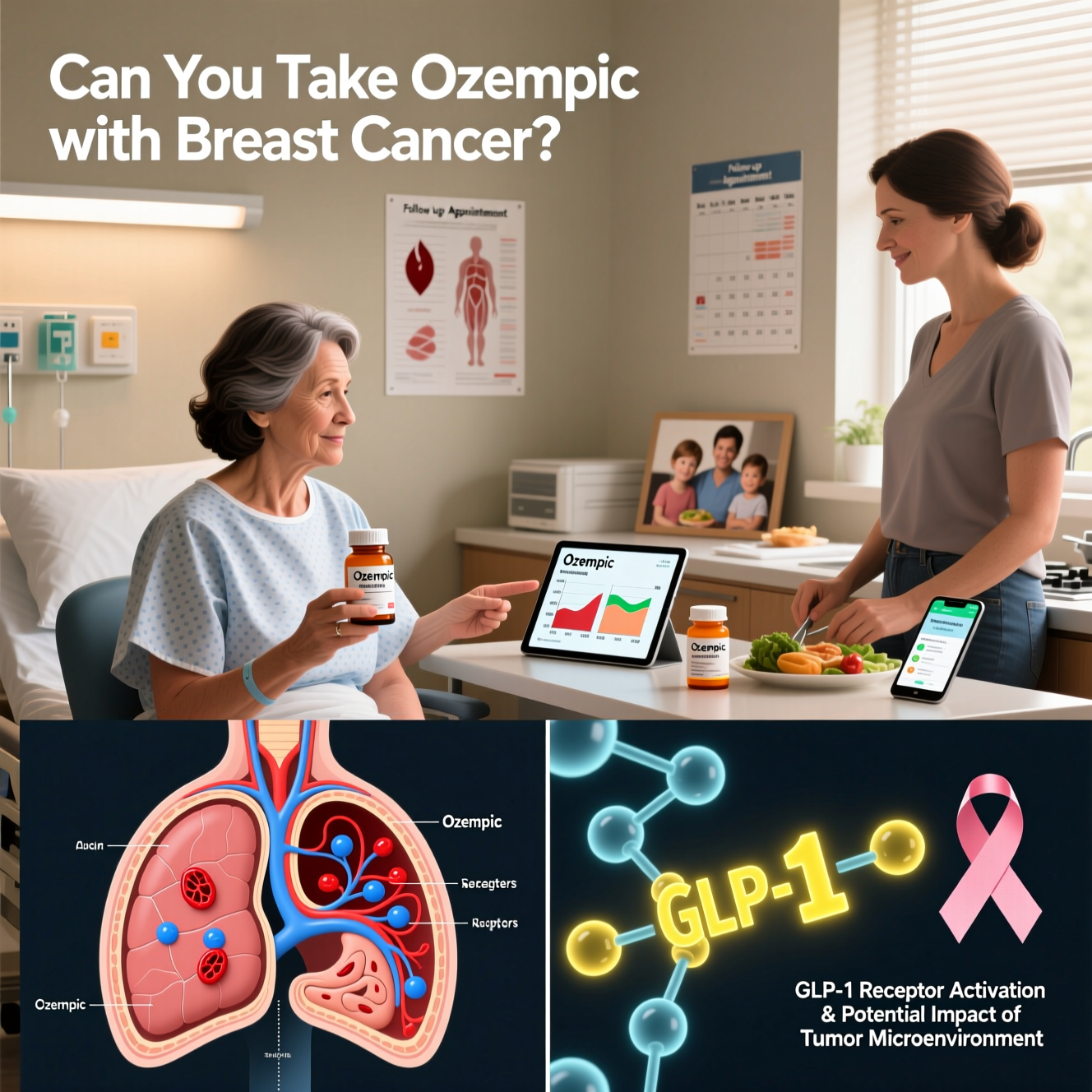
The intersection of GLP-1 medications and cancer care represents an evolving area of medical research. Several studies are investigating whether these drugs could play a role in cancer prevention or treatment.
Leading cancer centers, including Memorial Sloan Kettering Cancer Center, are conducting studies to determine whether weight loss medications like Ozempic should be recommended for cancer patients and survivors. Early findings suggest potential benefits, but researchers emphasize the need for comprehensive long-term data.
Some studies are exploring whether the metabolic improvements from GLP-1 agonists could create less favorable environments for cancer cell growth. Obesity-related inflammation, insulin resistance, and hormonal imbalances create conditions that can promote tumor development, and addressing these factors might offer protective benefits. Additionally, researchers are investigating whether these medications could help prevent cancer in high-risk populations, such as obese individuals or those with metabolic syndrome—conditions strongly linked to increased cancer risk.
Working With Your Healthcare Team
If you’re a breast cancer patient or survivor considering Ozempic, the decision should involve comprehensive discussions with your medical team, including your oncologist, endocrinologist, and primary care physician.
Before starting semaglutide therapy, discuss several important points with your healthcare providers. Understanding where you are in your cancer journey—active treatment, surveillance, or long-term survivorship—is crucial, as your treatment phase significantly influences whether GLP-1 therapy is appropriate. Your doctor will perform a thorough risk-benefit analysis to determine if your personal situation warrants the potential benefits of weight loss and improved metabolic health against any theoretical risks.
Exploring alternative options is also important. Are there other weight management strategies or medications that might be more suitable for your specific circumstances? Your healthcare team will also outline what additional testing or follow-up would be necessary if you start this medication, and how Ozempic might interact with your current medications, including any ongoing cancer treatments or preventive therapies.
Personalized Treatment Considerations
Every cancer patient’s situation is unique, requiring personalized medical decision-making. Factors your healthcare team will consider include cancer type, stage, and hormone receptor status, as well as time since diagnosis and treatment completion. Your current weight and BMI (body mass index), presence of diabetes or prediabetes, and other comorbid conditions all play crucial roles in the decision-making process.
Your current medication regimen, family medical history, and personal preferences and treatment goals will also be evaluated comprehensively to ensure the best possible outcome for your individual circumstances.
Essential Lifestyle Modifications
Regardless of whether you use Ozempic or other weight loss medications, lifestyle modifications remain the cornerstone of health maintenance for cancer survivors. These interventions work synergistically with pharmacological treatments and sometimes eliminate the need for medication entirely.
Adopting a cancer-protective diet rich in vegetables, fruits, whole grains, lean proteins, and healthy fats supports weight management and may reduce recurrence risk. The Mediterranean diet pattern has shown particular promise in cancer survivorship research, with its emphasis on anti-inflammatory foods and balanced macronutrients. Focus on nutrient-dense foods that provide vitamins, minerals, and phytochemicals while controlling calorie intake. Limit processed foods, added sugars, and excessive red meat consumption—dietary factors associated with increased cancer risk.
Regular exercise offers numerous benefits for cancer survivors, including weight control, improved strength and energy, reduced fatigue, better mood, and potentially lower recurrence risk. Aim for at least 150 minutes of moderate-intensity aerobic activity weekly, plus strength training exercises twice per week. Physical activity also improves insulin sensitivity, reduces inflammation, and optimizes hormone levels—all factors relevant to breast cancer outcomes and overall health.
Chronic stress and poor sleep quality can sabotage weight management efforts and potentially impact cancer outcomes through hormonal and immune system effects. Incorporate stress-reduction techniques like meditation, yoga, or mindfulness practices, and prioritize adequate sleep (7-9 hours nightly).
Alternative Weight Management Options
If Ozempic isn’t appropriate for your situation, several alternatives exist for weight management in breast cancer patients and survivors.
Other GLP-1 receptor agonists like Wegovy (higher-dose semaglutide specifically approved for weight loss), Saxenda (liraglutide), and Mounjaro (tirzepatide) offer similar mechanisms with some variations in efficacy, side effects, and dosing schedules. Non-GLP-1 weight loss medications include Contrave (naltrexone/bupropion), Qsymia (phentermine/topiramate), and Xenical (orlistat). Each has distinct mechanisms, benefits, and risks that should be discussed with your healthcare provider.
Structured weight loss programs, working with registered dietitians, behavioral therapy, and support groups can achieve significant weight loss without medications. These approaches are often recommended as first-line treatments, with medications added if needed. For individuals with severe obesity and cancer history, bariatric surgery might be considered after careful evaluation of risks and benefits in the context of cancer survivorship.
Monitoring Requirements and Follow-Up Care
If you and your healthcare team decide that Ozempic is appropriate, regular monitoring ensures safe and effective use. Regular blood work to check glucose levels, kidney function, and thyroid function is essential. Tracking weight and body composition helps monitor progress toward healthy weight goals, while evaluating gastrointestinal tolerance and overall wellbeing ensures the medication isn’t causing problematic side effects.
Continuing recommended screening and follow-up protocols for cancer recurrence remains paramount, as does ensuring adequate calorie and nutrient intake despite appetite suppression. Seek immediate medical attention if you experience severe abdominal pain (which could indicate pancreatitis), persistent vomiting, signs of thyroid tumors (neck mass, difficulty swallowing, persistent hoarseness), or any concerning new symptoms.
Making an Informed Decision
Taking Ozempic with breast cancer is not strictly contraindicated, but it requires careful consideration and medical supervision. Current evidence doesn’t suggest that semaglutide increases breast cancer risk or interferes with breast cancer treatment, though research in this specific population remains limited.
For many breast cancer survivors, particularly those struggling with weight gain and metabolic issues after treatment, GLP-1 receptor agonists might offer valuable benefits. However, the decision must be individualized based on cancer status, treatment phase, overall health, and personal circumstances.
The most important step is open communication with your oncology team. Together, you can weigh the potential benefits of improved weight management and metabolic health against any theoretical risks, ensuring your treatment plan aligns with your overall cancer care strategy and long-term health goals.
As research continues to evolve in this area, we’ll gain better understanding of how these powerful medications fit into comprehensive cancer care. Until then, decisions should be made collaboratively between patients and their healthcare providers, with careful monitoring and attention to both oncologic and metabolic health priorities.
Remember that medication is just one tool in the broader context of cancer survivorship care. Prioritizing evidence-based lifestyle modifications, maintaining regular follow-up care, and staying informed about your health remain the foundation of successful long-term outcomes after breast cancer.

Lisa Caldwell is a clinical health writer and certified diabetes educator with a strong background in pharmacology and metabolic health. With over 12 years of experience in patient education, she specializes in translating complex research on GLP-1 medications like Ozempic into clear, practical guidance.