Ozempic, the superstar medication fueled by semaglutide, has swept the health world with its dual powers of managing type 2 diabetes and driving impressive weight loss. From celebrity endorsements to social media buzz, it’s no wonder people are clamoring to get their hands on this weekly injection. But for those eyeing Ozempic to shed pounds rather than control blood sugar, a burning question looms: Will Anthem, one of the largest health insurers in the U.S., cover it for weight loss? As a medical and insurance expert, I’ll unravel the complexities of Anthem’s coverage policies, dive into the science, and offer practical tips for navigating this tricky terrain. Let’s embark on this journey with optimism and a clear-eyed look at the facts.
Understanding Ozempic and Its Weight Loss Appeal
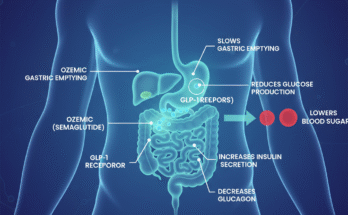
Ozempic is a GLP-1 receptor agonist, a class of drugs that mimics a hormone to regulate blood sugar, slow digestion, and curb appetite. Approved by the FDA for type 2 diabetes management and reducing cardiovascular risk in diabetic patients with heart disease, Ozempic has a side effect that’s caught everyone’s attention: significant weight loss. Clinical trials, like those in the SUSTAIN program, showed patients losing 10-15% of their body weight, sparking its off-label use for obesity. This off-label buzz has made Ozempic a go-to for those seeking weight loss, but insurance coverage hinges on FDA-approved indications, and that’s where things get murky with Anthem.
Anthem’s Coverage Landscape: The Basics
Anthem Blue Cross Blue Shield, part of Elevance Health, operates across multiple states, offering a range of plans with varying coverage rules. For medications like Ozempic, coverage depends on the specific plan, the patient’s diagnosis, and whether the drug is prescribed for an FDA-approved use. Anthem typically covers Ozempic for type 2 diabetes when prescribed with proper documentation, such as proof of diagnosis, prior treatment attempts (like metformin), and often a prior authorization to confirm medical necessity. However, when it comes to weight loss, Anthem’s stance is stricter. Most Anthem plans do not cover Ozempic for weight loss alone, as it’s considered an off-label use, not approved by the FDA for obesity management. This distinction is critical, as insurers like Anthem prioritize FDA indications to control costs and ensure evidence-based prescribing.
Why the Weight Loss Coverage Gap?
The reluctance to cover Ozempic for weight loss stems from a mix of regulatory and economic factors. Ozempic’s FDA approval is limited to type 2 diabetes and cardiovascular risk reduction, while its cousin, Wegovy—also semaglutide—is approved for weight management in adults with obesity (BMI ≥30) or overweight (BMI ≥27) with weight-related conditions like hypertension. Anthem is more likely to cover Wegovy for weight loss, provided patients meet strict criteria, such as a documented BMI and evidence of failed lifestyle interventions like diet and exercise for at least six months. However, even Wegovy coverage isn’t guaranteed, as some Anthem plans exclude weight loss drugs entirely due to their high cost—often exceeding $1,000 per month. A 2024 lawsuit in Maine highlighted Anthem’s “obesity exclusion” clause, which blocks coverage for drugs like Ozempic when prescribed solely for weight loss, leaving patients to pay out of pocket or seek alternatives.
Recent Shifts: A Glimmer of Hope?
In a promising development, Anthem has started to loosen its stance for specific cases. In 2024, Elevance Health announced that Anthem would cover Wegovy for certain Medicare and commercial plan members with cardiovascular disease to reduce heart attack and stroke risk, following new FDA approval for this indication. While this doesn’t directly apply to Ozempic, it signals a willingness to cover GLP-1 agonists for broader health benefits beyond diabetes. For weight loss, though, Anthem’s policies remain restrictive. Some plans may cover Ozempic off-label for weight loss if a provider can demonstrate medical necessity, such as prediabetes or weight-related comorbidities, but this requires robust documentation and often an appeal process. Social media posts on X and Reddit threads reflect patient frustration, with many reporting denials for Ozempic weight loss prescriptions under Anthem plans, underscoring the challenge of securing coverage.
Navigating the Coverage Maze
If you’re hoping to get Ozempic covered by Anthem for weight loss, preparation is key. Start by confirming your plan’s formulary, a list of covered drugs accessible via Anthem’s website or by calling the Pharmacy Member Services number on your ID card. Check if Ozempic or Wegovy is included and under what conditions. For weight loss, ask your doctor to explore prescribing Wegovy instead, as its FDA approval for obesity increases the odds of coverage. Ensure your medical records document a BMI ≥30 (or ≥27 with conditions like hypertension) and prior attempts at lifestyle changes, as Anthem often requires this for Wegovy approval. Prior authorization is almost always needed, so your provider must submit evidence of medical necessity, including lab results or weight-related health issues. If coverage is denied, don’t lose hope—file an appeal with additional documentation, as persistence can sometimes overturn denials.
Alternatives and Cost-Saving Strategies
When Anthem denies Ozempic for weight loss, patients have options. Wegovy, if covered, is the most direct alternative, though it’s pricier and still subject to strict criteria. Other GLP-1 agonists, like Saxenda (liraglutide) or Mounjaro (tirzepatide), may be covered under certain plans, so discuss these with your doctor. Novo Nordisk, Ozempic’s manufacturer, offers a savings card for eligible patients with commercial insurance, potentially reducing costs to as little as $25 for a 1-3 month supply, though this applies only to type 2 diabetes prescriptions. Without insurance, Ozempic’s list price hovers around $935-$1,029 monthly, making patient assistance programs or manufacturer discounts critical. Some patients turn to compounded semaglutide from specialty pharmacies, which can be cheaper but lack FDA approval and carry risks. Always consult your doctor before exploring non-FDA-approved options.
The Bigger Picture: Why Coverage Matters
The debate over covering Ozempic for weight loss isn’t just about cost—it’s about health equity and long-term outcomes. Obesity is linked to serious conditions like heart disease, diabetes, and joint issues, and drugs like Ozempic could reduce these risks, potentially saving insurers money over time. Critics argue that Anthem’s restrictive policies, like the “obesity exclusion” clause, limit access to transformative treatments, especially for those who can’t afford to pay out of pocket. A 2024 article from The Wall Street Journal noted that insurers like Anthem are beginning to cover Wegovy for cardiovascular benefits, hinting at a shift toward recognizing the broader health impacts of weight loss drugs. As research evolves, Anthem may expand coverage if data shows cost-effectiveness in preventing obesity-related complications.
FAQs
1. Why won’t Anthem cover Ozempic for weight loss?
Anthem typically denies Ozempic for weight loss because it’s not FDA-approved for this use, only for type 2 diabetes and cardiovascular risk reduction. Most plans view weight loss as an off-label use, and Anthem’s policies often exclude coverage for non-FDA-approved indications. Wegovy, approved for weight management, may be covered if you meet specific criteria like a high BMI and documented lifestyle interventions.
2. Can I appeal an Anthem denial for Ozempic coverage?
Yes, you can appeal a denial by submitting additional documentation through your healthcare provider. Include evidence of medical necessity, such as a high BMI, weight-related health issues, or failed prior treatments. Check your denial letter for specific reasons and follow Anthem’s appeal process, which is outlined on their website or in your plan documents.
3. Are there cheaper alternatives to Ozempic for weight loss if Anthem won’t cover it?
If Anthem denies Ozempic, ask your doctor about Wegovy or Saxenda, which may be covered for weight loss under certain conditions. Novo Nordisk’s savings card can lower Ozempic costs for type 2 diabetes prescriptions. Compounded semaglutide is another option, but it’s not FDA-approved, so discuss risks with your provider.
Conclusion
Anthem’s coverage of Ozempic for weight loss is a tough nut to crack, with most plans limiting it to type 2 diabetes due to FDA restrictions and cost concerns. While Wegovy offers a better shot at coverage for obesity, strict criteria and prior authorizations still apply. By understanding your plan, working closely with your doctor, and exploring appeals or assistance programs, you can improve your chances of accessing this game-changing drug. As insurers like Anthem grapple with the rising demand for GLP-1 agonists, future policy shifts may open doors, but for now, persistence and savvy navigation are your best allies. Stay proactive, and don’t let the insurance maze dim your health goals.

James Rowen is a certified medical writer and healthcare researcher specializing in endocrinology and metabolic health. With over a decade of experience analyzing weight management therapies, James has developed deep expertise in GLP-1 receptor agonists, including Ozempic.