Ozempic has become the talk of the town, not just for managing type 2 diabetes but for its jaw-dropping weight loss results. If you’re a Kaiser Permanente member eyeing this injectable wonder drug to shed pounds, you’re probably asking: Does Kaiser cover Ozempic for weight loss? As a healthcare expert, I’m here to cut through the confusion with a clear, engaging guide to Kaiser’s policies, costs, and your options. The answer isn’t straightforward—it hinges on your plan, region, and medical needs. Let’s unravel the details and empower you to navigate this process like a pro.
Understanding Ozempic’s Appeal
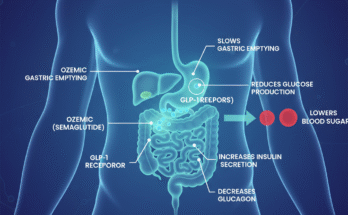
Ozempic, known generically as semaglutide, is a glucagon-like peptide-1 (GLP-1) receptor agonist. Approved by the FDA in 2017 for type 2 diabetes, it helps regulate blood sugar by mimicking a hormone that boosts insulin production and curbs appetite. This appetite-suppressing effect is why Ozempic has become a weight loss superstar, even when prescribed off-label. Clinical trials show users can lose 15% of their body weight on average—think 30 pounds for a 200-pound person. That’s life-changing for many struggling with obesity. But here’s the rub: a single 2mg/3ml pen, roughly a month’s supply, costs about $1,351 without insurance. For Kaiser Permanente’s 12 million-plus members, coverage is the golden ticket. So, what does Kaiser say?
Kaiser’s Coverage for Ozempic: Diabetes vs. Weight Loss
Kaiser Permanente, one of America’s largest not-for-profit health plans, generally covers Ozempic for its FDA-approved purpose: managing type 2 diabetes. If you have a confirmed diabetes diagnosis, your doctor can prescribe Ozempic, typically after you’ve tried other medications like metformin without success. Kaiser often requires prior authorization, meaning your provider must submit clinical records proving medical necessity. For diabetes, Ozempic is usually listed as a tier 3 drug in Kaiser’s 2025 Comprehensive Formulary, so expect copays or coinsurance based on your plan. If you’re losing weight as a side effect of diabetes treatment, that’s a happy bonus, but coverage is tied to the diabetes diagnosis, not weight loss goals.
When it comes to using Ozempic solely for weight loss, things get murkier. Since Ozempic isn’t FDA-approved for this purpose, it’s considered an off-label use, and coverage varies by region and plan. In Kaiser’s Northwest region, covering states like Oregon and Washington, you’re more likely to get coverage for weight loss if you meet strict criteria. These include a body mass index (BMI) of 30 or higher (or 27 with conditions like hypertension or sleep apnea) and participation in a Kaiser weight management program, which might involve diet counseling, exercise plans, or behavioral therapy. Your doctor will also need to secure prior authorization, documenting that other weight loss methods have failed.
In contrast, Kaiser members in California face tougher restrictions. Starting January 1, 2025, Kaiser Permanente’s commercial plans in California will no longer cover GLP-1 drugs like Ozempic for weight loss in patients with a BMI under 40. This change reflects rising costs and demand for these medications. If you’re in California and seeking Ozempic for weight loss without a diabetes diagnosis, you might be out of luck unless your BMI is significantly high or you have specific health conditions. Other regions, like Colorado or Hawaii, follow similar patterns, with coverage depending on your plan’s formulary and whether you’ve enrolled in a structured weight management program. Always check your plan’s Evidence of Coverage document on kp.org for specifics.
Exploring Wegovy and Other Alternatives
If Kaiser won’t cover Ozempic for weight loss, don’t lose hope. Wegovy, another semaglutide drug from Novo Nordisk, is FDA-approved for chronic weight management and may be covered under some Kaiser plans. Wegovy has similar eligibility requirements—BMI of 30 or higher (or 27 with comorbidities), prior authorization, and often participation in a weight management program. Since it’s FDA-approved for weight loss, you might have an easier time getting coverage for Wegovy than Ozempic in some regions. However, it’s still a tier 3 drug, so costs like copays apply. Other weight loss medications, such as phentermine/topiramate (Qsymia) or bupropion/naltrexone (Contrave), might also be covered and could be more affordable options. Discuss these with your doctor to see what aligns with your health goals and plan.
Managing Costs Without Coverage
If Kaiser denies coverage for Ozempic or Wegovy, the out-of-pocket price—around $1,351 monthly for Ozempic—can feel like a punch to the wallet. Fortunately, there are ways to soften the blow. Novo Nordisk offers an Ozempic Savings Card, which can shave $100 off a one-month supply for those with partial private insurance coverage. Their patient assistance program may help if you meet income criteria. SingleCare coupons, available online, can sometimes reduce the cost to under $1,000 per month. If you’re enrolled in Kaiser’s Medical Weight Management Program, you might be able to use pre-tax dollars from a Flexible Spending Account (FSA) or Health Savings Account (HSA) to cover costs. For those exploring non-Kaiser options, telehealth services can prescribe Ozempic and have it filled through Kaiser’s mail-order pharmacy, potentially at a discount. Always compare prices and check for manufacturer discounts before paying full retail.
Tips to Navigate Kaiser’s System
Getting Ozempic covered for weight loss requires strategy and persistence. Start by logging into kp.org to review your plan’s formulary or call Kaiser’s customer service to confirm coverage details. Next, schedule a visit with your primary care provider or an endocrinologist. Be honest about your weight loss goals and medical history—conditions like insulin resistance or sleep apnea can strengthen your case. Many Kaiser plans require you to join a weight management program, such as their Medical Weight Management Program, which includes virtual classes, meal replacements, and regular check-ins. In Southern California, for example, you may need to complete a 90-minute virtual weight loss class before seeing a specialist. If Kaiser denies coverage, don’t give up. File an appeal with additional medical documentation or request a peer-to-peer review between your doctor and Kaiser’s team. A health advocate can guide you through this process if it feels daunting.
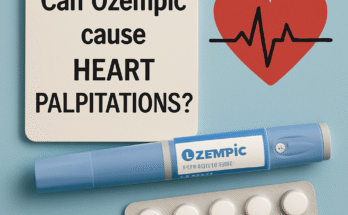
Weighing the Pros and Cons of Ozempic
Ozempic’s weight loss benefits are impressive, but it’s not a one-size-fits-all solution. Common side effects include nausea, vomiting, and diarrhea, and there’s a rare risk of thyroid tumors. Weight loss often plateaus, and stopping the drug can lead to weight regain if lifestyle changes aren’t maintained. Kaiser emphasizes a holistic approach—diet, exercise, and behavioral therapy—as the cornerstone of sustainable weight loss, with medications like Ozempic as a supplement. Before committing, consider whether the potential $700–$1,300 monthly cost (even with discounts) is worth the 20–90 pounds you might lose. For some, it’s a game-changer; for others, Kaiser’s weight management programs or alternative drugs may be more practical.
Frequently Asked Questions
What documentation do I need to get Ozempic covered for weight loss?
To get Ozempic covered for weight loss, Kaiser typically requires a BMI of 30 or higher (or 27 with conditions like hypertension), proof of failed attempts at other weight loss methods, and enrollment in a Kaiser weight management program. Your doctor must submit a prior authorization request with medical records, including your BMI, health conditions, and a history of lifestyle interventions.
Can I appeal a denial of Ozempic coverage?
Yes, you can appeal a denial by submitting additional documentation, such as detailed medical records or a letter from your doctor explaining why Ozempic is medically necessary. You can also request a peer-to-peer review, where your provider discusses your case with Kaiser’s medical team. Contact Kaiser’s customer service or a health advocate for guidance.
Is Wegovy a better option than Ozempic for weight loss coverage?
Wegovy, being FDA-approved for weight loss, may have a higher chance of coverage than Ozempic in some Kaiser plans. However, it still requires prior authorization, a qualifying BMI, and often participation in a weight management program. Check your plan’s formulary to compare coverage details.
Conclusion
So, does Kaiser Permanente cover Ozempic for weight loss? It’s possible, but it depends on your plan, region, and whether you meet strict criteria like BMI thresholds and program participation. Northwest members have a better shot, while California members face new restrictions in 2025. Check your plan’s formulary, work closely with your doctor, and explore alternatives like Wegovy or cost-saving options like manufacturer discounts. Weight loss is a journey, and with the right approach—whether it’s Ozempic, a Kaiser program, or lifestyle changes—you can find a path that works for you. For more details, visit kp.org or contact Kaiser’s customer service.
Jake Morrison is a health journalist and certified medical researcher who specializes in obesity treatment and diabetes care. With a background in biomedical science and years spent analyzing real-world outcomes of GLP-1 therapies like Ozempic, Jake brings an evidence-driven, reader-friendly approach to complex medical topics.