You’re scrolling through Reddit at 2 AM, chest burning like you just chugged hot sauce, wondering if your new Ozempic prescription is the culprit. Sound familiar? You’re not alone – and you’re not imagining things.
As a board-certified nurse practitioner who’s managed hundreds of patients on GLP-1 therapies, I’ve fielded this question more times than I can count. The short answer? Yes, Ozempic can cause acid reflux. But here’s the thing – understanding why it happens and what you can do about it makes all the difference between suffering through it and managing your health like a pro.
Let’s discuss Ozempic and acid reflux in detail because your gut deserves better than guesswork.
The Real Connection: Why Ozempic Messes With Your Stomach
Here’s where things get interesting from a clinical standpoint. Ozempic doesn’t just randomly decide to torch your esophagus – there’s actual science behind why this happens.
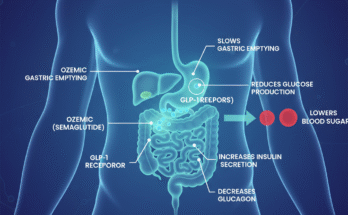
The Gastric Emptying Game-Changer
Ozempic works by mimicking GLP-1, a hormone that’s like your body’s natural appetite control system. But here’s the kicker – it also slows down how fast your stomach empties. Think of it like traffic during rush hour. When food sits in your stomach longer, pressure builds up, and things start backing up into your esophagus.
I’ve seen this play out countless times in my practice. Patients come in describing that “burning sensation” or feeling like food is just sitting there like a rock. That’s your stomach saying, “Hey, we’re backed up here.”
The Pressure Cooker Effect
When gastric emptying slows down, intragastric pressure increases. Your stomach becomes like an overpacked suitcase – eventually, something’s got to give. That “something” is often your lower esophageal sphincter (LES), the muscle that’s supposed to keep stomach acid where it belongs.
Some research suggests that GLP-1 agonists might even relax this sphincter, making reflux more likely. It’s like having a bouncer who’s suddenly decided to take a nap on the job.
The Numbers Don’t Lie: How Common Is Ozempic-Related Reflux?
Let’s talk data, because I believe in giving you the straight facts. Clinical trials show that about 2% of patients report heartburn or acid reflux, with higher rates in those taking the 0.5 mg weekly dose. But here’s what those numbers don’t capture – the real-world experience often tells a different story.
What the Trials Actually Show
In the STEP 1-3 trials, 72.9% of participants on semaglutide 2.4 mg reported GI symptoms, compared to 47.1% in the placebo groups. The most common complaints included:
- Nausea (43.9%)
- Diarrhea (29.7%)
- Vomiting (24.5%)
- Constipation (24.2%)
But here’s where it gets interesting – acid reflux often flies under the radar in these studies because it’s not always the primary complaint. Patients might describe “stomach upset” or “indigestion” without specifically mentioning that burning chest sensation.
The Postmarketing Reality Check
Since Ozempic hit the market, the FDA’s Adverse Event Reporting System has logged 223 cases of impaired gastric emptying and 149 intestinal obstructions as of December 2023. Many of these cases included reflux-like symptoms, painting a clearer picture of what’s actually happening out there.
Timing Is Everything: When Reflux Strikes
From my clinical experience, acid reflux typically shows up during two key periods:
The Honeymoon Phase (Weeks 1-4)
Most patients experience their worst GI symptoms during the initial dose-escalation phase. Your body is basically learning how to work with this new medication, and things can get messy. The good news? These symptoms often resolve within a few weeks as your system adjusts.
The Dose-Bump Drama
Every time you increase your Ozempic dose, you’re essentially restarting this adjustment period. I always warn my patients that they might experience a resurgence of symptoms, including reflux, with each dose increase.
Red Flags: When Reflux Becomes Dangerous
Here’s where my clinical alarm bells start ringing. While most Ozempic-related reflux is manageable, certain symptoms require immediate medical attention:
The “Oh Crap” Symptoms
- Hematemesis (vomiting blood) or melena (black, tarry stools)
- Unexplained weight loss beyond your target goals
- Dysphagia (difficulty swallowing)
- Persistent vomiting that won’t quit
- Severe abdominal distention
These could signal serious complications like gastroparesis or even intestinal obstruction. The FDA updated Ozempic’s label in September 2023 to include warnings about ileus and gastroparesis for exactly this reason.
The Gastroparesis Connection
Here’s something that keeps me up at night as a clinician – the risk of gastroparesis. A JAMA study found that GLP-1 users had a 3.67-fold higher risk of gastroparesis compared to other weight-loss medications. When your stomach essentially stops working properly, reflux becomes the least of your worries.
Your Action Plan: Managing Ozempic-Related Reflux Like a Pro
Alright, enough doom and gloom. Let’s talk solutions. After years of helping patients navigate this, I’ve developed a pretty solid playbook for managing Ozempic-related reflux.
The Food Strategy That Actually Works
Forget everything you think you know about “diet advice.” Here’s what actually moves the needle:
The 2-Hour Rule: Stay upright for at least two hours after eating. I don’t care if Netflix is calling – gravity is your friend here.
Size Matters: Smaller, more frequent meals are your new best friend. Think tapas, not Thanksgiving dinner.
The Trigger Food Hit List: High-fat, spicy, or acidic foods are basically asking for trouble. That doesn’t mean you can never have pizza again, but timing and portion control become crucial.
The Medication Backup Plan
Sometimes lifestyle changes aren’t enough, and that’s okay. Here’s what I typically recommend:
Proton Pump Inhibitors (PPIs): Short-term use of medications like omeprazole can provide significant relief. I emphasize short-term because long-term PPI use comes with its own set of concerns.
Antiemetics: For severe nausea and vomiting, medications like ondansetron can be game-changers. Don’t suffer through it – there are solutions.
Dose Adjustment Strategy: Sometimes slower titration is the answer. Instead of following the standard dosing schedule, we might extend intervals between dose increases to improve tolerability.
The Science Behind the Suffering: Understanding GLP-1’s Double-Edged Sword
Let’s get nerdy for a minute because understanding the mechanism helps you make better decisions about your health.
The GLP-1 Receptor Agonist Explanation
Ozempic works by activating GLP-1 receptors throughout your body, not just in your pancreas. These receptors are found in your stomach, intestines, and even your brain. When activated, they:
- Enhance insulin secretion (the diabetes benefit)
- Suppress glucagon release (more blood sugar control)
- Slow gastric emptying (the satiety effect that also causes problems)
- Signal fullness to your brain (appetite suppression)
The problem is that you can’t cherry-pick these effects. The same mechanism that helps with weight loss and blood sugar control also slows down your digestive system.
The Motility Disruption
Your gastrointestinal tract is like a well-choreographed dance. When Ozempic disrupts this rhythm by slowing gastric emptying, it affects the entire sequence. Food sits longer in your stomach, pressure builds, and your esophageal motility can also be affected.
Some patients describe a sensation of food “sticking” or burning in their chest – that’s often altered esophageal motility at work.
Monitoring and Management: Your Long-Term Strategy
Here’s where my clinical experience comes into play. Managing Ozempic-related reflux isn’t just about treating symptoms – it’s about preventing complications and optimizing your overall health outcomes.
The Monitoring Schedule That Works
Weeks 1-4: Weekly check-ins (virtual or in-person) to assess symptom progression and adjust management strategies.
Monthly assessments: Once you’re stable, monthly monitoring helps catch any emerging issues before they become serious.
Dose increase periods: Extra vigilance during dose escalations, with specific attention to GI symptoms.
The Hydration Game-Changer
Here’s something that doesn’t get enough attention – proper hydration. Clear, non-carbonated fluids aid digestion and can help prevent the constipation that often compounds reflux issues.
But here’s the catch – timing matters. Drinking large amounts of fluid with meals can actually worsen reflux by increasing gastric volume. Sip throughout the day, but go easy during meals.
The Future of GLP-1 Therapy: What’s Coming Next
As someone who stays plugged into the latest research, I’m excited about what’s on the horizon for GLP-1 therapies. Preliminary studies suggest that chronic GLP-1 agonist use might alter gut microbiota composition, potentially influencing GI motility and acid secretion.
Researchers are also investigating dual GLP-1/FGF21 receptor agonists that might mitigate some of the GI side effects we see with current medications. The goal is to maintain the metabolic benefits while reducing the digestive disruption.
Your Personalized Approach: Making Ozempic Work for You
Here’s the thing – medicine isn’t one-size-fits-all, and neither is managing Ozempic-related reflux. What works for your friend might not work for you, and that’s completely normal.
The Individual Assessment
When I evaluate patients for Ozempic-related reflux, I consider:
Baseline GI health: Do you have a history of GERD, gastroparesis, or other digestive issues?
Medication timing: Are you taking Ozempic with other medications that might affect gastric emptying?
Lifestyle factors: Stress, sleep patterns, and eating habits all play a role.
Dose progression: How quickly are we escalating your dose, and how is your body responding?
The Collaborative Approach
Managing Ozempic successfully requires teamwork between you and your healthcare provider. Don’t just tough it out – communicate what you’re experiencing. We can’t help what we don’t know about.
FAQ’s
What is the biggest side effect of Ozempic?
Nausea is the most common Ozempic side effect. Still, not everyone has it. About 1 in 5 people in the clinical trial had it. Nausea is usually mild to moderate and at its worst when you first start the drug or when you increase your dose.
What settles acid reflux immediately?
Once acid reflux starts, you can use over-the-counter medications, like antacids or H2 blockers, to stop the symptoms fast. Home remedies, like drinking milk or eating a banana, may also help relieve heartburn symptoms. If medications don’t relieve your heartburn, you may need medical care.
How long does acid reflux last with Ozempic?
If your symptoms aren’t getting better within 2 weeks, talk with a healthcare professional about prescription options. Ozempic-related heartburn does go away on its own, but this can take a few weeks. Treatment can keep you comfortable while you wait.
How do you stop acid reflux on Ozempic?
Try an over-the-counter reflux medication
Antacids: Tums, Rolaids, Alka-Seltzer, and Mylanta. These work quickly to neutralize stomach acid and provide immediate relief, but their effects are short-lived.
The Bottom Line: Balancing Benefits and Side Effects
Does Ozempic cause acid reflux? Absolutely. But does that mean you should avoid it? That depends on your situation and how well you can manage the side effects.
In my practice, I’ve seen patients successfully navigate Ozempic-related reflux by:
- Understanding the mechanism behind their symptoms
- Implementing targeted lifestyle modifications
- Using appropriate medications when needed
- Maintaining open communication with their healthcare team
- Staying vigilant for red flag symptoms
The key is finding that sweet spot where you’re getting the metabolic benefits of Ozempic while minimizing the digestive disruption. It’s possible – you just need the right strategy and support.
Remember, your health journey is unique. What matters most is working with a healthcare provider who understands both the benefits and risks of GLP-1 therapy and can help you navigate them safely.
Your gut health matters, your metabolic health matters, and finding the right balance between the two is what good medicine is all about.
Emily Harper is a board-certified nurse practitioner and certified obesity medicine specialist with a strong clinical background in metabolic health and GLP-1 therapies. With years of frontline experience managing patients on Ozempic, she brings both scientific knowledge and real-world insight to her writing.