You’re scrolling through Reddit at 2 AM (again), and there it is – another thread about Ozempic making people “pee out sugar.” Your prescription bottle’s sitting on the nightstand, and suddenly you’re wondering if your body’s turned into some kind of glucose fountain. I get it. This question lands in my inbox more than DMs from crypto bros, and honestly? It’s time we set the record straight.
After years of managing patients on GLP-1 medications, I’ve heard every concern, myth, and midnight panic Google search you can imagine. So let’s dive into what’s actually happening in your body when you’re on Ozempic – no medical jargon, no corporate speak, just the real deal.
The Short Answer: Nope, Ozempic Doesn’t Make You Pee Sugar
Here’s the thing – does ozempic make you pee out sugar? The straightforward answer is no. Ozempic (semaglutide) doesn’t work by making your kidneys dump glucose into your urine like some biological water feature. That’s not its game at all.
I’ve had patients come in convinced they’re literally peeing away their breakfast because they read something online or overheard a conversation at the gym. Last month, a 28-year-old tech worker spent three days tracking his urine with test strips because he was sure Ozempic was making him excrete sugar. Spoiler alert: it wasn’t.
Ozempic works through completely different mechanisms that have nothing to do with your kidneys playing glucose DJ.
How Ozempic Actually Works (Without the Textbook Drama)
Think of Ozempic as your body’s personal blood sugar bouncer. It doesn’t kick glucose out through the back door (your urine) – instead, it manages the whole party from the inside.
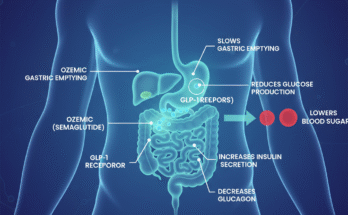
The Real MVP Moves
Insulin Gets Smarter: When you eat, Ozempic tells your pancreas, “Hey, time to release insulin, but only when we actually need it.” No more random insulin drops that leave you hangry and confused.
Glucagon Takes a Chill Pill: Your liver usually loves dumping stored glucose into your bloodstream like it’s Black Friday. Ozempic tells it to relax and stop the glucose fire sale.
Your Stomach Hits the Brakes: Food moves through your system slower, which means no more blood sugar roller coaster after meals. Think of it as your digestive system switching from Formula 1 to a nice Sunday drive.
I had a patient describe it perfectly: “It’s like my body finally learned how to use an indoor voice instead of screaming about every piece of food I ate.”
But Wait – Why Do People Think It Makes Them Pee Sugar?
The confusion is real, and it’s not coming from nowhere. Here’s where things get interesting.
The Diabetes Connection
If you’re managing type 2 diabetes and your blood sugar was previously sky-high, you might have been experiencing glycosuria – that’s when your kidneys actually do dump excess glucose into your urine because your blood sugar levels are off the charts.
Here’s the plot twist: when Ozempic gets your blood sugar under control, you might actually pee out less sugar than before. Your kidneys can finally take a break from working overtime.
The Bathroom Frequency Factor
You might be hitting the bathroom more often on Ozempic, but it’s not because you’re peeing out sugar. A few things are actually happening:
Hydration Station: We tell patients to drink more water to combat those initial GI side effects. More water in, more trips to the bathroom – basic math.
Early Adjustment Phase: Your body’s recalibrating its glucose game, which can temporarily affect fluid balance while everything settles.
Weight Loss Effects: As you drop weight, your body composition changes, and yes, that can affect bathroom habits too.
The Real Urinary Changes You Might Notice
Now, this is where my clinical experience gets interesting. While Ozempic doesn’t make you pee out sugar, some patients do notice other changes that are worth discussing.
Stress Incontinence – The Plot Twist Nobody Saw Coming
Here’s something that caught even me off guard initially: rapid weight loss from Ozempic can lead to stress incontinence. Your pelvic floor muscles, which were used to supporting a certain body weight, suddenly find themselves in a different situation.
I had a 32-year-old patient who lost 40 pounds in six months and started experiencing leakage when she laughed or sneezed. The connection between rapid weight loss and weakened pelvic floor muscles is real, but it’s manageable with the right approach.
The Smell Test
Some patients mention changes in urine odor – not because of sugar, but likely due to altered gut bacteria or slower digestion affecting how waste is processed. Your gut microbiome is basically getting a renovation, and sometimes that comes with temporary side effects.
What Your Kidneys Are Actually Doing on Ozempic
Plot twist: Ozempic might actually be your kidneys’ new best friend. The research here is pretty compelling, and it’s one of the reasons I’m genuinely excited about this medication class.
The Protection Game
Studies show GLP-1 agonists like Ozempic can reduce kidney disease progression by 24% in type 2 diabetes patients. We’re talking anti-inflammatory effects, antioxidant properties, and reduced protein spillage into urine.
For someone like me who’s seen too many patients progress to dialysis, this protective effect is huge. Your kidneys aren’t just not being harmed – they’re potentially being helped.
The Risk Reality Check
That said, there’s one scenario where kidney problems can occur: severe dehydration from nausea and vomiting. If you’re so nauseated that you can’t keep fluids down, acute kidney injury becomes a possibility. This is rare, but it’s why we monitor kidney function closely, especially in the first few months.
Monitoring Your Health Like a Pro
Here’s your practical game plan – the stuff I actually tell my patients, not the generic advice you’ll find everywhere else.
Blood Work That Matters
Every 3-6 Months: HbA1c and fasting glucose – these tell us how your average blood sugar is trending over time.
Baseline and Periodic: Kidney function tests (eGFR, serum creatinine) and lipid profiles. I usually check these every 6 months unless there’s a specific concern.
Symptom Tracking That’s Actually Useful
Instead of obsessing over whether you’re peeing out sugar (you’re not), track things that actually matter:
Urinary Changes: Frequency, urgency, any incontinence, or significant odor changes Hydration Status: Are you drinking enough water? Your urine color is a better indicator than any fancy app GI Symptoms: Nausea, vomiting, or anything that might affect your fluid intake
| Monitoring Schedule | What to Check | Why It Matters |
| Weekly | Urine color, bathroom frequency | Early dehydration detection |
| Monthly | Weight, energy levels, GI symptoms | Overall treatment response |
| Every 3-6 months | Blood work, kidney function | Long-term health tracking |
When to Actually Worry (And When You’re Just Overthinking)
I’ve learned to distinguish between legitimate concerns and 3 AM Google spiral symptoms. Here’s your reality check.
Red Flags That Need Attention
Severe Dehydration: If you’re so nauseated you can’t keep fluids down for more than 24 hours Sudden Changes: Dramatic shifts in urination patterns, especially with pain or burning Kidney Function Decline: This shows up in blood work, not symptoms you can feel
Normal Stuff That Freaks People Out
Increased thirst initially: Your body’s adjusting to better blood sugar control Slight changes in bathroom frequency: Especially if you’re drinking more water Temporary urine odor changes: Usually resolves as your system adapts
FAQ’s
Is blood in urine a side effect of Ozempic?
Kidney problems – swelling, urinating less, blood in urine, feeling tired or short of breath. stomach flu symptoms – stomach cramps, vomiting, loss of appetite, diarrhea (may be watery or bloody)
What medication makes you pee out sugar?
Empagliflozin works by helping your body to remove extra sugar through your pee. Your doctor may recommend empagliflozin for treating type 2 diabetes if: diet and exercise are not enough to control your blood sugar levels. you cannot take metformin (another type of diabetes medicine)
Does Ozempic get rid of sugar?
It works by helping your body to produce more insulin when needed. It also reduces the amount of glucose, or sugar, produced by the liver, and slows down how quickly food is digested. This all helps to lower blood sugar levels and HbA1c.
Does Ozempic make you pee more sugar?
Does Ozempic make you pee more? Ozempic may not increase your urination but can alter your urine output depending on your health condition. People with hyperglycemia experience an urge for high thirst and frequent urination. Ozempic helps reduce symptoms related to kidney disease
The Bottom Line From Someone Who’s Seen It All
After managing hundreds of patients on Ozempic, here’s what I want you to know: the whole “peeing out sugar” thing is a myth that needs to die. Your kidneys aren’t turning into glucose fountains, and you’re not literally flushing away your health.
What Ozempic actually does is far more sophisticated – it helps your body remember how to manage blood sugar like it did before everything went sideways. The urinary changes people notice are usually related to weight loss, hydration changes, or the body’s adjustment period.
The evidence suggests Ozempic might actually protect your kidneys long-term, which is the opposite of what the internet panic would have you believe.
Your Next Steps (No Panic Required)
If you’re currently on Ozempic and worried about urinary changes, here’s your action plan:
Stay hydrated – seriously, this solves like 80% of the concerns I see. Track any significant changes in bathroom habits, but don’t obsess over normal fluctuations. Keep up with your regular blood work to monitor kidney function and overall health.
And remember – if something feels genuinely off, that’s what your healthcare provider is for. We’ve seen it all, and trust me, your questions aren’t as weird as you think they are.
The goal isn’t perfect health – it’s informed health. You’ve got the knowledge now. Time to put those 2 AM Google sessions to rest and focus on the real benefits this medication can offer.
Want to dive deeper into GLP-1 medications and their real-world effects? Check out our other posts on managing Ozempic side effects and optimizing your treatment journey.
Emily Harper is a board-certified nurse practitioner and certified obesity medicine specialist with a strong clinical background in metabolic health and GLP-1 therapies. With years of frontline experience managing patients on Ozempic, she brings both scientific knowledge and real-world insight to her writing.