When beginning treatment with Ozempic (semaglutide), one of the most common questions patients ask is how long the medication stays in their system and how it actually works to manage blood sugar levels and promote weight loss. Understanding the half-life of Ozempic and its mechanism of action can help you better appreciate why this once-weekly injection has become a cornerstone treatment for type 2 diabetes and obesity management.
What Is Half-Life and Why Does It Matter?
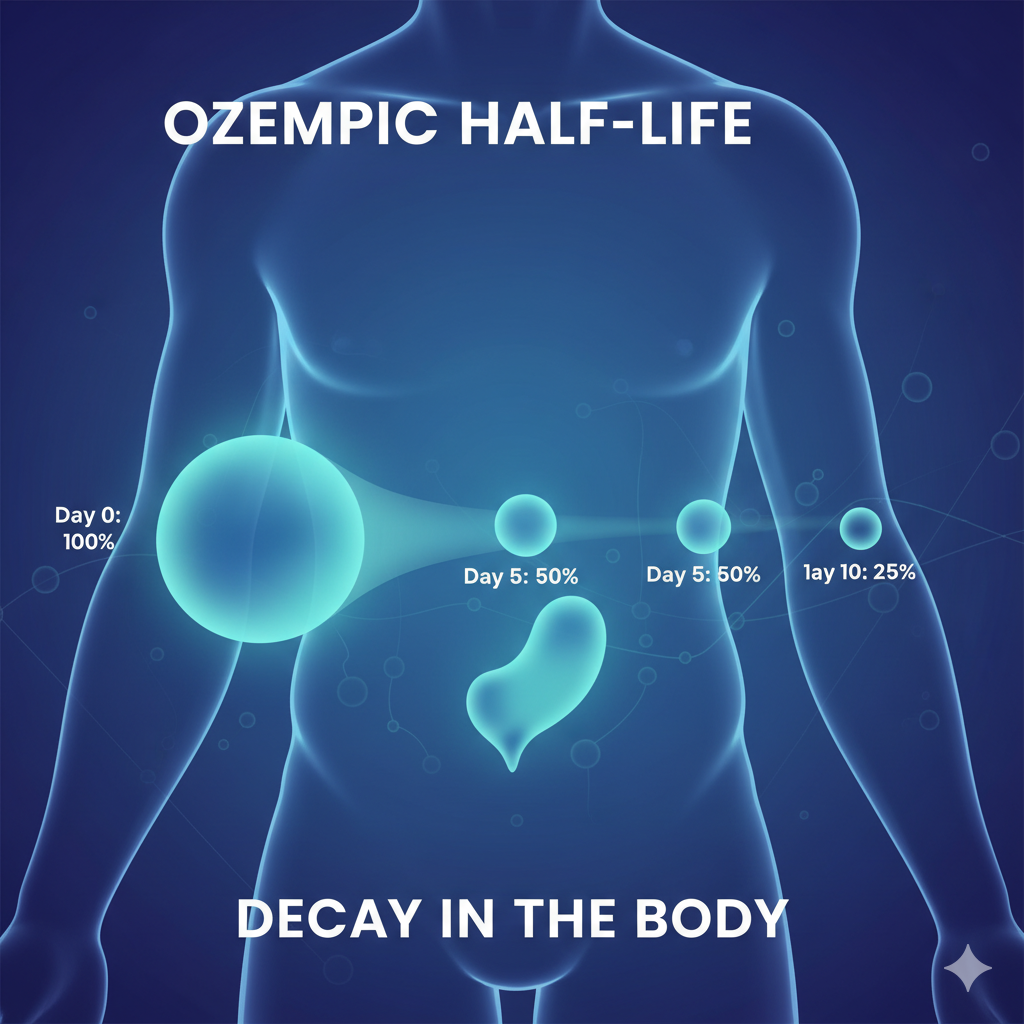
Before diving into Ozempic specifically, it’s essential to understand what drug elimination half-life means. The half-life of a medication refers to the time it takes for half of the drug to be eliminated from your bloodstream. This pharmacokinetic property determines how often you need to take a medication and how long its effects last in your body.
Semaglutide has an elimination half-life of approximately one week, meaning the medication remains present in circulation for about five weeks after the last dose. This extended duration is precisely why Ozempic can be administered as a once-weekly injection rather than daily, offering significant convenience compared to many other diabetes medications.
The Science Behind Semaglutide Half-Life Duration
The extended semaglutide half-life is not accidental—it’s the result of sophisticated pharmaceutical engineering. Semaglutide is structurally designed to resist rapid breakdown in the body through several key modifications. The molecule includes a fatty acid side chain that allows it to bind to albumin, a protein abundant in blood plasma. This albumin binding semaglutide characteristic protects the medication from quick degradation and extends its time in circulation.
Additionally, specific amino acid substitutions in the peptide structure make semaglutide resistant to an enzyme called DPP-4 (dipeptidyl peptidase-4), which normally breaks down natural GLP-1 hormones within minutes. These modifications transform what would be a hormone lasting only a few minutes into a long-acting diabetes medication that remains effective for an entire week.
How Does Ozempic Work for Weight Loss and Blood Sugar Control?
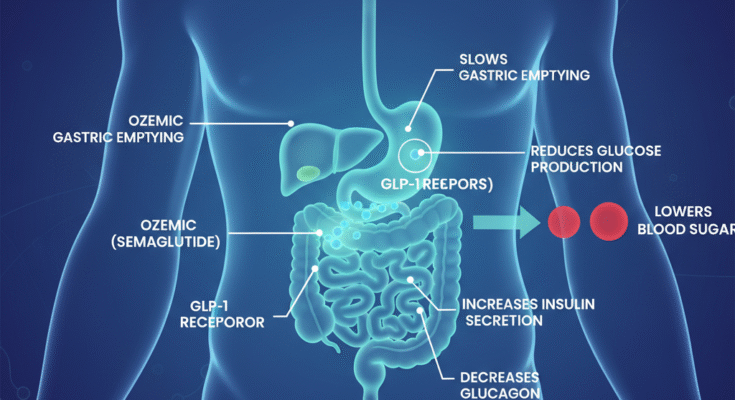
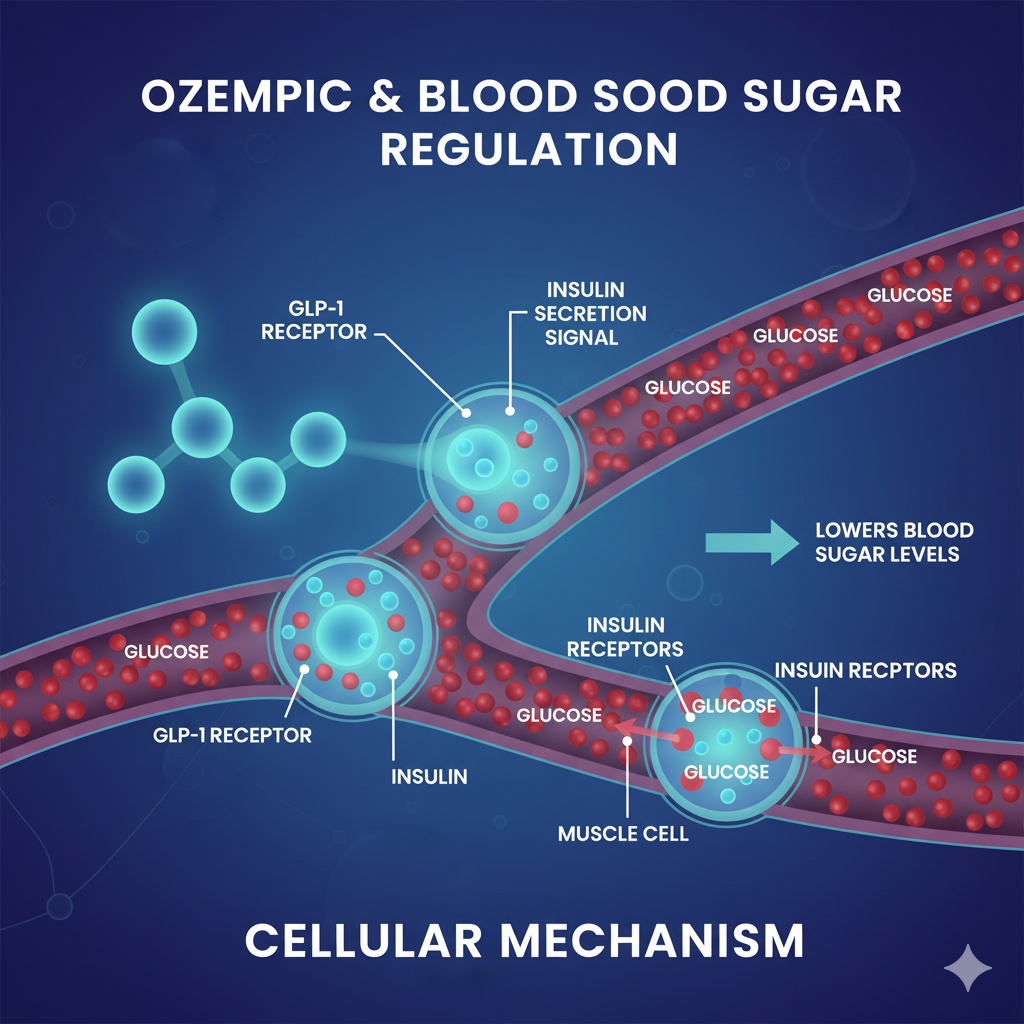
Ozempic belongs to a class of medications called GLP-1 receptor agonists, also known as incretin mimetics or GLP-1 mimetic function drugs. To understand how Ozempic works, you first need to know about GLP-1 (glucagon-like peptide-1), a natural incretin hormone produced in your intestines after eating.
The GLP-1 Receptor Agonist Mechanism
The semaglutide mechanism of action mimics and enhances the effects of natural GLP-1 in multiple ways:
Insulin Secretion Enhancement: When you eat, Ozempic increases insulin secretion from your pancreas in response to meals, which helps lower blood sugar levels. Importantly, this insulin release is glucose-dependent, meaning it primarily occurs when blood sugar levels are elevated, reducing the risk of hypoglycemia compared to some other diabetes medications.
Glucagon Suppression: By binding to GLP-1 receptors in the pancreas, semaglutide suppresses the release of glucagon, a hormone that raises blood sugar. This dual action—increasing insulin while decreasing glucagon—creates a powerful effect on blood glucose regulation.
Gastric Emptying Delay: One of the most significant ways Ozempic affects the body is by slowing stomach emptying, which means slower digestion and less rapid glucose release from food into the bloodstream. How Ozempic slows gastric emptying contributes both to improved blood sugar control and the sensation of fullness that aids weight loss.
Appetite Reduction: GLP-1 affects brain regions that process hunger and satiety, increasing how full you feel after eating. This appetite-suppressing effect is a primary reason how does Ozempic work for weight loss beyond its metabolic effects.
Ozempic Pharmacokinetics: Absorption and Distribution
Understanding Ozempic pharmacokinetics helps explain why the medication is so effective and convenient. After subcutaneous injection (under the skin), the medication undergoes a complex journey through your body.
Ozempic Absorption and Metabolism
The Ozempic bioavailability subcutaneous route is approximately 89%, meaning nearly 90% of the injected dose reaches systemic circulation. This high bioavailability is one reason why subcutaneous administration is so effective for this peptide drug.
After injection, semaglutide is slowly and steadily absorbed into the bloodstream. Maximum concentration in the blood typically occurs 1-3 days after injection, but the medication continues to work throughout the week due to its prolonged presence in circulation.
Distribution and Protein Binding
Once in the bloodstream, semaglutide distributes throughout the body with a volume of distribution of approximately 12.5 liters. The extensive albumin binding—over 99% of semaglutide molecules attach to this blood protein—contributes significantly to the extended half-life and protects the medication from rapid elimination.
How Long Does It Take for Ozempic to Work?
Patients often ask, “how long does it take for Ozempic to work?” The answer depends on what effects you’re measuring:
Blood Sugar Effects: You may notice improvements in blood sugar levels within the first week of treatment as the medication begins accumulating in your system. However, maximum glucose-lowering effects typically develop over several weeks as you reach steady-state concentrations.
Steady State Concentration: The time to reach steady state Ozempic is approximately 4-5 weeks of weekly injections. At steady state, the amount of medication being eliminated equals the amount being added with each dose, creating consistent therapeutic levels in your bloodstream. This is why healthcare providers typically wait at least one month before increasing your dose.
Weight Loss Timeline: Weight reduction effects generally become noticeable after 4-8 weeks of treatment, with continued weight loss occurring over several months as you progress through dose escalation.
Ozempic Dosing Schedule and Titration
The standard Ozempic dosing schedule involves gradual dose escalation:
Initial Dose: Treatment begins with 0.25 mg once weekly for four weeks. This starting dose primarily helps your body adjust to the medication and minimizes gastrointestinal side effects.
Ozempic 0.25 mg to 0.5 mg Transition: After four weeks, most patients increase to 0.5 mg weekly. This is considered the first therapeutic dose for blood sugar control.
Further Increases: When to increase Ozempic dose depends on your blood sugar control and treatment goals. If additional glucose lowering is needed, your healthcare provider may increase the dose to 1 mg weekly after at least four weeks at 0.5 mg. Some patients may eventually progress to 2 mg weekly for maximum effect.
The gradual titration is essential for tolerability and allows your body to adapt to the medication’s effects, particularly regarding gastric emptying and appetite changes.
Why Is Ozempic Injected Once Weekly?
The once-weekly injection schedule is possible specifically because of the extended semaglutide half-life duration and favorable pharmacokinetic properties. While natural GLP-1 hormones are degraded within minutes of release, semaglutide’s modifications allow it to persist for days.
The long plasma half-life of approximately one week combined with steady dosing results in reduced variability of medication exposure at steady state. This means your medication levels remain relatively stable throughout the week, even though you’re only injecting once every seven days.
This Ozempic weekly injection duration offers significant advantages over daily injections, improving treatment adherence and quality of life for patients managing chronic conditions.
How Long Does Ozempic Stay in Your System?
Given the approximately one-week half-life, you might wonder: how long does Ozempic stay in your system after stopping treatment?
With an elimination half-life of approximately one week, semaglutide will be present in circulation for about five weeks after the final dose. This extended Ozempic clearance from body timeline has several important implications:
Ozempic Discontinuation Timeline: If you stop taking Ozempic, therapeutic effects will gradually diminish over 4-5 weeks as the medication is eliminated. Blood sugar levels may begin rising within 1-2 weeks, though some appetite suppression and gastric emptying effects may persist longer.
Missing Ozempic Dose Effects: If you miss a single dose, significant medication levels remain in your system from previous injections. Your healthcare provider can advise whether to take the missed dose or wait until the next scheduled injection, depending on timing.
Ozempic Washout Period Before Surgery: Healthcare providers typically recommend discontinuing Ozempic before certain surgical procedures due to its gastric emptying effects. The complete Ozempic washout period is approximately 5 weeks, though specific recommendations depend on the type of surgery planned.
How Long After Stopping Ozempic Do Side Effects Last: Most side effects, particularly gastrointestinal symptoms, gradually improve as medication levels decline over the 4-5 week clearance period.
Ozempic Pharmacodynamics Explained
While pharmacokinetics describes what your body does to the medication, pharmacodynamics explains what the medication does to your body. Understanding Ozempic pharmacodynamics helps clarify how long therapeutic effects persist.
The effects on pancreas function—specifically insulin secretion enhancement and glucagon suppression—correlate closely with medication levels in the blood. As semaglutide concentrations rise to peak levels 1-3 days after injection, these effects are maximized. They remain strong throughout the week due to sustained medication presence.
The gastric emptying delay and appetite effects follow a similar pattern but may have slightly longer-lasting impacts on behavior and eating patterns, even as medication levels begin to decline toward the end of the dosing interval.
Comparing Semaglutide to Other GLP-1 Medications
Understanding how Ozempic compares to other GLP-1 medications list options can help contextualize its unique properties:
Semaglutide vs Liraglutide Half-Life: Liraglutide (Victoza) has a much shorter half-life of approximately 13 hours, requiring daily injection. The extended semaglutide half-life represents a significant advancement in peptide drug pharmacokinetics.
Dulaglutide Half-Life vs Semaglutide: Dulaglutide (Trulicity) is also a once-weekly GLP-1 agonist with a half-life of approximately 5 days. While both are weekly injections, semaglutide’s slightly longer half-life and higher potency at receptors may contribute to its robust efficacy.
Exenatide Weekly vs Ozempic: Extended-release exenatide (Bydureon) requires weekly injection, but its pharmacokinetic profile differs substantially from semaglutide due to its microsphere delivery system rather than structural modifications.
Tirzepatide vs Semaglutide Comparison: Tirzepatide (Mounjaro) is actually a dual GIP/GLP-1 receptor agonist with a half-life of approximately 5 days. The Mounjaro mechanism of action includes both GLP-1 and GIP receptor activation, potentially offering additional metabolic benefits, though direct comparisons continue in ongoing research.
Wegovy vs Ozempic: Same Medication, Different Purpose
A common question is: “Is Wegovy the same as Ozempic?” The answer is yes—both contain semaglutide with identical pharmacokinetics and mechanism of action. The difference lies in dosing and FDA-approved indications:
- Ozempic: Approved for type 2 diabetes, maximum dose 2 mg weekly
- Wegovy: Approved for weight management, maximum dose 2.4 mg weekly
The higher Wegovy dose leverages semaglutide’s appetite-suppressing and gastric emptying effects for dedicated weight loss treatment in individuals with obesity or overweight with weight-related conditions.
Oral Semaglutide: A Different Delivery Method
Rybelsus Absorption Compared to Ozempic: Oral semaglutide (Rybelsus) represents a significant pharmaceutical achievement—delivering a peptide hormone orally despite poor natural bioavailability. Rybelsus uses a special absorption enhancer called SNAC to facilitate uptake in the stomach.
Oral Semaglutide vs Injectable: While both formulations contain the same active ingredient with similar half-lives, oral semaglutide bioavailability is much lower (approximately 1% compared to 89% for subcutaneous injection). This necessitates daily administration and higher nominal doses. However, the convenience of a pill versus injection appeals to many patients despite lower bioavailability.
Practical Implications of Ozempic’s Half-Life
Understanding peptide drug metabolism and specifically how Ozempic’s extended half-life affects treatment has several practical applications:
Consistency Is Key: The weekly injection schedule works because steady-state concentrations maintain therapeutic effects between doses. Consistency in injection timing optimizes stability of medication levels.
Dose Adjustments Require Patience: Because it takes 4-5 weeks to reach new steady-state levels after dose changes, allow adequate time before adjusting again. Premature dose increases may lead to higher medication levels than intended and increased side effects.
Transition Planning: If switching from Ozempic to another GLP-1 medication, the 5-week clearance period means overlapping effects are possible. Your healthcare provider will plan transition timing accordingly.
Managing Side Effects: If gastrointestinal side effects occur, remember they typically improve over time as your body adapts. Since medication accumulates over the first month, side effects may be minimal initially but increase as you approach steady state.
Safety Considerations and Monitoring
The extended time semaglutide remains in your system requires awareness of certain safety considerations:
Drug Interactions: The gastric emptying delay can affect absorption of oral medications. Take Ozempic consistently and monitor the effectiveness of other medications, particularly those with narrow therapeutic windows.
Surgical Planning: Inform surgical teams about Ozempic use. The 5-week clearance period may influence timing of elective procedures where delayed gastric emptying poses risks.
Hypoglycemia Risk: While Ozempic alone rarely causes low blood sugar due to its glucose-dependent mechanism, combining it with insulin or sulfonylureas increases hypoglycemia risk. Dose adjustments of these medications may be necessary.
The Future of Long-Acting GLP-1 Medications
Ozempic represents a significant advancement in incretin-based therapy, demonstrating how pharmaceutical engineering can transform a naturally occurring hormone lasting minutes into a once-weekly medication. The success of semaglutide has spurred continued research into long-acting diabetes medications and next-generation GLP-1 therapies.
Understanding the glucagon-like peptide-1 function and how modifications create extended half-lives has opened pathways for developing other peptide-based therapies with improved pharmacokinetic profiles. Future medications may offer even longer dosing intervals or enhanced selectivity for specific therapeutic effects.
Conclusion: Making the Most of Ozempic’s Unique Properties
The approximately one-week half-life of Ozempic is fundamental to its effectiveness and convenience as a treatment for type 2 diabetes and obesity. This extended duration allows once-weekly dosing while maintaining stable therapeutic effects throughout the week.
By understanding how semaglutide works—from its GLP-1 receptor agonist activity to its effects on insulin secretion, glucagon suppression, gastric emptying, and appetite—patients can better appreciate how this medication addresses multiple aspects of metabolic dysfunction simultaneously.
Whether you’re considering starting Ozempic, currently using it, or simply interested in how modern diabetes medications work, understanding the pharmacokinetics, pharmacodynamics, and mechanism of action of semaglutide provides valuable insight into one of the most significant therapeutic advances in metabolic medicine.
Remember that while this article provides comprehensive information about how Ozempic works in the body, always consult your healthcare provider for personalized medical advice regarding your specific treatment plan. Your provider can help determine the appropriate Ozempic dosing schedule, monitor your response to therapy, and adjust treatment as needed to achieve optimal outcomes.
For those seeking additional information, consulting Ozempic FDA label information, Novo Nordisk semaglutide clinical data, and the Ozempic patient information leaflet can provide detailed prescribing information and safety data specific to your needs.
Emily Harper is a board-certified nurse practitioner and certified obesity medicine specialist with a strong clinical background in metabolic health and GLP-1 therapies. With years of frontline experience managing patients on Ozempic, she brings both scientific knowledge and real-world insight to her writing.