If you’re scheduled for an upcoming surgical procedure and currently taking Ozempic (semaglutide), understanding when to stop this medication is crucial for your safety. The question of how long to stop semaglutide before an operation has become increasingly important as GLP-1 medications like Ozempic, Wegovy, and Mounjaro have grown in popularity for diabetes management and weight loss.
Recent medical guidelines have established clear protocols regarding GLP-1 medications and surgery guidelines, primarily due to concerns about delayed gastric emptying and potential complications during anesthesia. This comprehensive guide will walk you through everything you need to know about stopping Ozempic before general anesthesia, managing your diabetes during this period, and safely resuming treatment after your procedure.
Why Ozempic and Anesthesia Risks Require Special Attention
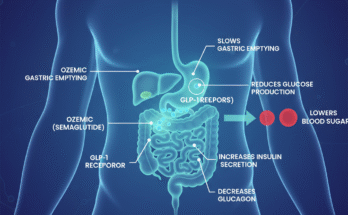
Semaglutide belongs to a class of medications called GLP-1 receptor agonists, which work by slowing gastric emptying to help control blood sugar and promote satiety. While this mechanism is beneficial for diabetes management and weight loss, it creates specific challenges during surgical procedures.
The primary concern centers on Ozempic gastric emptying surgery complications. When your stomach empties more slowly than normal, food and liquids may remain in your digestive system longer than expected—even after following standard pre-operative fasting protocols. This delayed gastric emptying significantly increases the potential for pulmonary aspiration prevention surgery complications.
During general anesthesia, your body’s protective reflexes are suppressed. If stomach contents are present when you’re under anesthesia, there’s a risk of regurgitation and aspiration—meaning stomach contents could enter your lungs. This complication, known as aspiration pneumonia, can be serious and potentially life-threatening. The Ozempic aspiration risk during surgery has prompted medical societies to issue updated recommendations for patients taking these medications.
Official GLP-1 Agonists Pre-Operative Fasting Guidelines

Medical organizations, including anesthesiology societies, have established specific protocols for patients on GLP-1 receptor agonists. Understanding these pre-operative medication management diabetes guidelines is essential for anyone scheduled for elective surgery and diabetes medication hold procedures.
The Standard Semaglutide Withdrawal Period Surgery Protocol
For most patients taking Ozempic, the recommended timeline is:
Weekly Dosing (Standard Ozempic): Discontinue the medication at least one week (7 days) before your scheduled surgery. However, many anesthesiologists and surgeons now recommend extending this to two weeks for added safety, particularly for major procedures requiring general anesthesia.
Daily GLP-1 Medications: For drugs like Victoza (liraglutide) with shorter half-lives, discontinuation 24-48 hours before surgery may be sufficient, though your medical team will provide specific guidance.
The question “is 7 days enough to stop Ozempic before surgery?” depends on several factors, including your dosage, how long you’ve been taking the medication, and the type of surgery planned. Recent evidence suggests that the semaglutide pharmacokinetics and surgery considerations may require longer discontinuation periods for some patients.
Do I Need to Stop Ozempic Before a Colonoscopy?
This is one of the most frequently asked questions. The answer is typically yes. Even for procedures involving moderate sedation like colonoscopies, most gastroenterologists now recommend stopping Ozempic for at least one week prior. The risk of full stomach surgery complications applies to any procedure requiring sedation, not just major operations.
Pre-Surgical Ozempic Taper Schedule and Clearance Requirements
Working with your healthcare team to develop a personalized pre-surgical Ozempic taper schedule is crucial. This process typically involves coordination between multiple specialists.
Your Ozempic Surgery Clearance Requirements Checklist
3-4 Weeks Before Surgery:
- Schedule an endocrinologist pre-op Ozempic consultation
- Discuss your complete medication list with your surgeon
- Obtain Ozempic surgical consent forms if required by your facility
- Review the anesthesiologist Ozempic protocol specific to your procedure
2 Weeks Before Surgery:
- Take your last dose of Ozempic (if following the conservative two-week protocol)
- Begin alternative diabetes medications before surgery if prescribed
- Monitor blood sugar levels more frequently
- Discuss managing blood sugar after stopping Ozempic strategies with your endocrinologist
1 Week Before Surgery:
- Confirm all pre-operative fasting instructions
- Understand specific NPO guidelines that diabetic patients must follow
- Final pre-surgical testing and clearances
- Review emergency contact information and post-operative care instructions
Day Before Surgery:
- Follow all fasting instructions precisely
- Check blood sugar levels as directed
- Prepare your post-surgical medication schedule
What Happens If I Don’t Stop Ozempic Before Surgery
The consequences of continuing Ozempic too close to your surgical date can be serious. Understanding what happens if I don’t stop Ozempic before surgery helps emphasize the importance of following medical advice.
Continuing GLP-1 medications without appropriate discontinuation increases your risk for:
Aspiration Pneumonia: The most serious concern. Ozempic stomach contents during anesthesia can lead to aspiration, where stomach contents enter the lungs. This can cause severe pneumonia, respiratory failure, and extended hospital stays.
Surgical Delays or Cancellations: Many anesthesiologists will postpone elective procedures if they discover patients are still actively taking Ozempic within the safety window. This can be frustrating and delay necessary treatment.
Extended NPO Periods: If surgery proceeds, you may face longer fasting requirements. Some facilities require patients who haven’t properly discontinued GLP-1 medications to undergo gastric emptying assessments before proceeding.
Increased Monitoring Requirements: Regurgitation risk Ozempic patients may need additional anesthesia monitoring, including potentially more aggressive airway management techniques.
Managing Blood Sugar Control Without Ozempic Surgery
One of the biggest concerns patients express is how to maintain glycemic control during the Ozempic discontinuation period. Fortunately, there are effective strategies for managing blood sugar after stopping Ozempic.
Alternative Diabetes Medications Before Surgery
Your endocrinologist may recommend temporary substitutions:
Short-Acting Insulin: Provides flexible blood sugar control that can be easily adjusted around surgical fasting requirements.
Metformin: May be continued or adjusted based on kidney function and surgical risks. Often held 48 hours before surgery involving contrast dye.
DPP-4 Inhibitors: Shorter-acting medications that work differently than GLP-1 agonists and don’t significantly affect gastric emptying.
SGLT-2 Inhibitors: May be continued or held depending on surgical type and hydration status.
Post-Prandial Gastroparesis Surgical Risk Management
For patients who have developed post-prandial gastroparesis from long-term GLP-1 use, additional precautions may be necessary. Your medical team might recommend:
- Upper GI studies to assess gastric emptying
- Extended medication washout periods
- Modified anesthesia approaches
- Clear liquid diets for several days before surgery
FDA Guidelines Ozempic Surgical Procedures and Official Recommendations
While the FDA hasn’t issued procedure-specific mandates, the ASMBS Ozempic surgery recommendations and other medical societies have established best practices. These guidelines continue to evolve as more clinical experience accumulates.
Recent updates emphasize:
Risk Stratification: Patients are categorized based on dosage, duration of use, and presence of gastroparesis symptoms.
Procedure Classification: Emergency surgery requires different management than elective procedures. For urgent operations, the benefits may outweigh aspiration risks, requiring enhanced airway protection strategies.
Communication Protocols: Clear documentation of GLP-1 use in pre-operative assessments and direct communication between prescribing physicians, surgeons, and anesthesiologists.
How Many Weeks Before Surgery Stop Ozempic: Individualized Timelines
The answer to “how many weeks before surgery stop Ozempic” isn’t one-size-fits-all. Several factors influence your specific timeline:
Dosage Considerations: Higher doses may require longer washout periods due to drug accumulation.
Treatment Duration: Patients on Ozempic for years may have more profound effects on gastric motility than those recently started.
Concurrent Medications: Other drugs affecting gastric emptying (opioids, anticholinergics) compound risks.
Type of Surgery: Major abdominal surgery, procedures requiring extended anesthesia, or operations in prone positioning carry higher aspiration risks.
Individual Physiology: Patient factors, including obesity, hiatal hernia, diabetes severity, and gastroparesis history, all influence recommendations.
When to Resume Ozempic After Surgery: Post-Operative Protocol
Understanding when to resume Ozempic after surgery is equally important as knowing when to stop. Your surgeon and endocrinologist will coordinate this decision based on several factors.
Typical Resumption Timeline
Minor Procedures (Outpatient, Local Anesthesia): May resume Ozempic within 24-48 hours if tolerating oral intake without nausea or vomiting.
Moderate Procedures (Same-Day Discharge, Moderate Sedation): Usually wait 3-5 days, ensuring normal oral intake and bowel function.
Major Surgery (Hospital Admission, General Anesthesia): Often wait 1-2 weeks, confirming stable nutrition, healing without complications, and approval from your surgical team.
Abdominal/GI Surgery: May require extended delays (2-4 weeks or longer) to ensure adequate healing and return of normal gastric function.
Signs You’re Ready to Restart GLP-1 Therapy
- Tolerating a regular diet without nausea or vomiting
- Normal bowel movements resumed
- Surgical wounds are healing appropriately
- No signs of infection or complications
- Clearance from your surgical team
- Stable blood sugar on interim medications
Special Considerations: Wegovy Surgery Discontinuation and Mounjaro Pre-Surgical Guidelines
While this article focuses primarily on Ozempic, patients on similar medications need comparable guidance.
Wegovy Surgery Discontinuation: Since Wegovy contains the same active ingredient as Ozempic (semaglutide), identical discontinuation timelines apply—typically 1-2 weeks before surgery.
Mounjaro Pre-Surgical Guidelines: Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist with similar gastric emptying effects. Current recommendations suggest discontinuing Mounjaro at least one week before surgery, with many experts recommending two weeks for major procedures.
Bariatric Surgery GLP-1 Receptor Agonists: Special Situations
Interestingly, patients undergoing bariatric surgery diabetes medication hold protocols face unique considerations. Many bariatric programs use GLP-1 medications as part of pre-surgical weight optimization. However, these must be carefully discontinued before the actual surgical procedure.
Post-bariatric surgery, GLP-1 medications may not be necessary initially due to hormonal changes from the surgery itself. Your bariatric team will determine if and when resuming these medications makes sense.
Can I Have Surgery While Taking Ozempic: Emergency Situations
In true emergency situations where surgery cannot be delayed, modifications to anesthesia management are made to minimize aspiration risks. This might include:
- Rapid sequence intubation techniques
- Cricoid pressure application
- Use of medications to increase gastric pH
- Enhanced airway protection measures
- Post-operative monitoring in intensive care settings
However, for elective surgery diabetes medication hold situations, proper discontinuation is always preferred.
Communicating with Your Surgical Team: Anesthesiologist Ozempic Protocol
Transparency with your medical team is paramount. During your pre-operative evaluation:
Provide Complete Medication History:
- Exact Ozempic dose and frequency
- Date of last injection
- Any missed doses or irregular administration
- All other medications, supplements, and over-the-counter drugs
Discuss Symptoms:
- Any ongoing nausea, bloating, or feeling of fullness
- Changes in appetite or digestion
- Previous issues with anesthesia or sedation
Ask Questions:
- Confirm specific discontinuation timeline for your situation
- Understand backup plans if surgery must be rescheduled
- Clarify post-operative medication restart protocols
Navigating Insurance and Documentation: Ozempic Surgical Consent Forms
Some medical facilities now require specific documentation regarding GLP-1 medication use. These Ozempic surgical consent forms typically include:
- Acknowledgment that you’ve been informed of aspiration risks
- Confirmation of medication discontinuation timeline
- Agreement to follow post-operative restrictions
- Understanding of potential complications
Completing these forms accurately ensures your entire care team has consistent information.
Practical Tips for the Discontinuation Period
Monitor Blood Sugar Closely: Check levels 3-4 times daily during the medication-free period, watching for unexpected highs or lows.
Maintain Hydration: Proper fluid intake supports healing and helps prevent constipation when transitioning between medications.
Eat Small, Frequent Meals: This can help maintain stable blood sugar without triggering nausea that sometimes occurs when discontinuing GLP-1 medications.
Keep a Symptom Journal: Track any unusual symptoms like increased hunger, blood sugar fluctuations, or digestive changes to discuss with your healthcare team.
Prepare Your Post-Surgery Environment: Stock healthy foods that align with both your diabetes management and post-surgical dietary requirements.
Conclusion: Prioritizing Safety Through Proper Planning
Understanding when to stop Ozempic before surgery and following medical guidelines for GLP-1 medications significantly reduces surgical risks. While discontinuing medication that helps manage your diabetes or weight may feel concerning, the temporary pause protects you from serious complications like aspiration pneumonia.
Work closely with your endocrinologist, surgeon, and anesthesiologist to develop a personalized plan that addresses your specific medical needs. By following proper Ozempic discontinuation before surgery timeline recommendations, maintaining communication with your healthcare team, and carefully managing your blood sugar during the transition period, you can safely navigate your surgical experience and resume your medication when appropriate.
Remember, every patient’s situation is unique. The information provided here serves as general guidance, but your individual treatment plan should be developed in consultation with your medical providers who understand your complete health picture. When in doubt, always err on the side of caution and communicate openly with your surgical team about any concerns.
The goal is successful surgery with optimal outcomes—and proper medication management is a crucial component of achieving that goal.

James Rowen is a certified medical writer and healthcare researcher specializing in endocrinology and metabolic health. With over a decade of experience analyzing weight management therapies, James has developed deep expertise in GLP-1 receptor agonists, including Ozempic.